Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 2 - Mar. / Apr. of 2007
Vol. 40 nº 2 - Mar. / Apr. of 2007
|
REVIEW ARTICLE
|
|
Three-dimensional ultrasound in gynecology: uterine malformations |
|
|
Autho(rs): Adilson Cunha Ferreira, Francisco Mauad Filho, Luis Guilherme Nicolau, Francisco M. Pancich Gallarreta, Wellington Martins de Paula, Débora Cristina Gomes |
|
|
Keywords: Uterine malformations, Müllerian malformations, Three-dimensional ultrasonography |
|
|
Abstract:
IPhD, Professors at EURP – Escola de Ultra-sonografia e Reciclagem Médica de Ribeirão Preto and Faculdade de Medicina de Ribeirão Preto (Unaerp), Ribeirão Preto, SP, Brazil
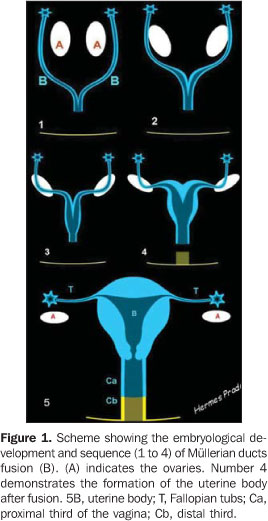
INTRODUCTION Uterine malformations are secondary to failure in development, reabsorption or fusion of Müllerian ducts. Around the sixth week of the embryogenesis, an invagination of the coelomic lining epithelium forms a depression creating a sulcus, whose borders fuse to form the lateral Müllerian ducts (or paramesonephric ducts) (Figure 1). The Müllerian ducts initially are formed in the upper dorsal wall of the coelomic cavity and progress caudally to enter the pelvis where they incline towards the center, fusing medially. Farther on, the caudal progress results in a contact of these fused ducts with the urogenital sinus. The proximal segments of the uterovaginal canal originated from coelomic epithelium remain unfused and open into the peritoneal cavity to form the Fallopian tubes. The upper portion of the vagina is, therefore, considered to have Müllerian origin, and the lower portion as originating from the urogenital sinus. He whole lining epithelium (uterus and tubes) originates from the coelomic epithelium. This is the reason for uterine malformations being denominated Müllerian malformations or anomalies(1).
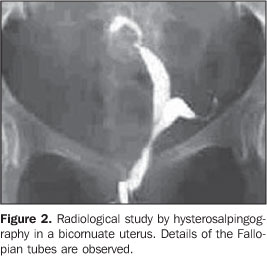
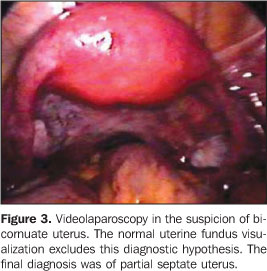
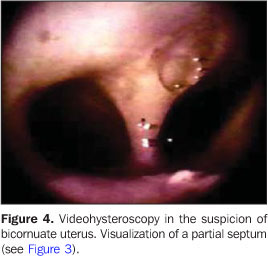
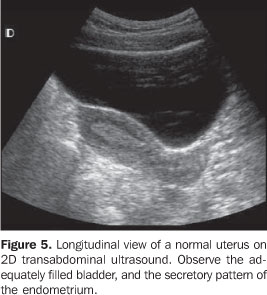
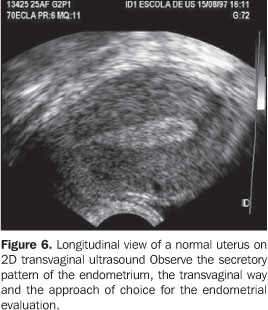
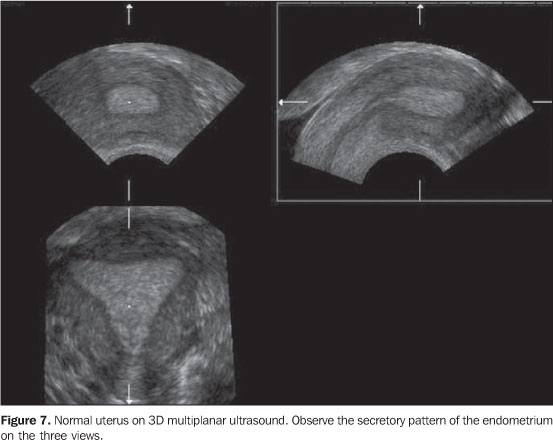
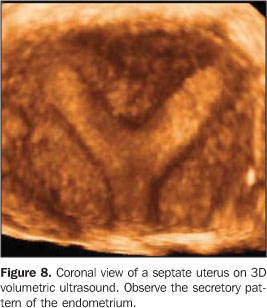
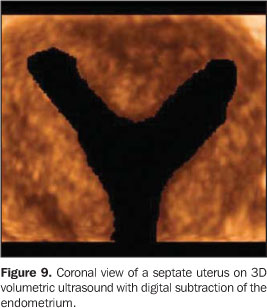
In the past, the uterus only could be clinically evaluated by means of a physical examination. Several methods have been introduced for gynecological evaluation. As an example, we can mention; radiological examinations(2) by means of hysterosalpingography(3–5) (Figure 2), surgical procedures — laparotomy, laparoscopy, and most recently, videolaparoscopy (Figure 3) — and hysteroscopy(6) (Figure 4). Undoubtedly, ultrasound is the method that has brought the greatest contribution as non-invasive method for evaluation of the uterus and its attachments(7), initially as a two-dimensional (2D) modality with an abdominal approach (Figure 5), and later with a transvaginal approach (Figure 6). Most recently, ultrasonography has been added of the three-dimensional (3D) processing(8–11) in both modalities — the multiplanar (Figure 7) and the volumetric ones (Figures 8, 9 and 10). Magnetic resonance imaging also has been utilized in many services(12).
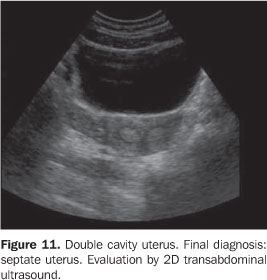
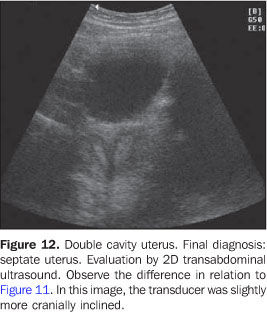
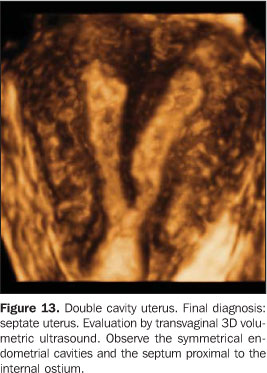
DISCUSSION Uterine malformations are unusual findings in thegynecological clinical practice. This abnormality is a reflectionof an array of presentations, associated with the fact that thediagnosis of the majority of malformations does not occur beforea gestation or are diagnosed only after manifestation of anobstetric problem(13–15). Statistics in thisarea are flawed, and there is a lack of standardization of thepertinent terminology, besides the difficulty in thediagnosis(16). Patients with these alterationsfrequently are oligosymptomatic or even asymptomatic, withpreserved menstrual, sexual and even reproductive functions. So,frequently presented case reports and casuistics reflectparticularities of certain groups of women with obstetriccomplications, patients of infertility and sterility services, orcases of medical urgency resulting from menstrual flowobstruction(17). Presently, 2D ultrasound, and especially 3D ultrasound areindispensable diagnostic tools for evaluation of uterinemalformations, allowing accurate diagnoses, most of times morespecific than a simple description of a septate uterus,characterizing the abnormality and providing information toassist in the definition of therapeutic regimen and reproductiveprognosis(18–21). The appropriate classification of Müllerian anomalies isimportant, the most relevant one being proposed by Jarcho in1946, and later adapted by Zanetti et al., based on the embryonaldevelopment. Later on, this classification was modified by Butramand Gibbons, in 1975, and is currently adopted by the AmericanSociety of Fertility. A better evaluation with 2D ultrasound is achieved by theassociation between transabdominal and transvaginal approaches.The first one allows a better visualization of the uterinefundus, and analysis of the bladder and ureteral jets. The secondallows a more detailed analysis of the cervix (cervices) andendometrial cavity (cavities). The main view for correctly diagnosing the type of themalformation is the coronal view, sometimes difficult to beobtained with the 2D technique, but feasible, provided sometechnical prerequisites are met: the bladder must be almostemptied; the transducer must be placed transversely to thepatient's abdomen with slight, cranial movements. Several anomalies may originate from an incomplete fusion the Müllerian ducts: clefts in the uterine funds, but not in the cervix, a complete division of the uterus by a septum into two endometrial cavities, forming the called septate uterus. The septum may be partial or complete, with variable extent from the uterine fundus towards the cervix (Figures 11, 12, 13, 14 and 15). Sometimes, the differential diagnosis with bicornuate uteri is difficult, especially if the sonographic evaluation is restricted to the transvaginal approach. Also, it may be associated with a longitudinal or oblique vaginal septum.
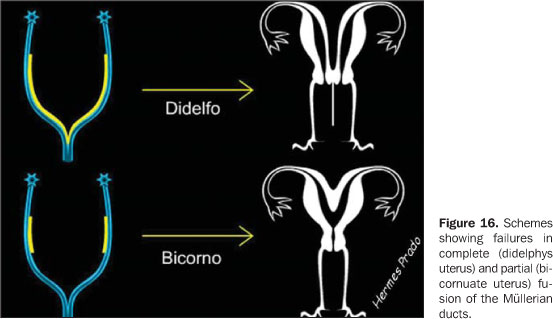
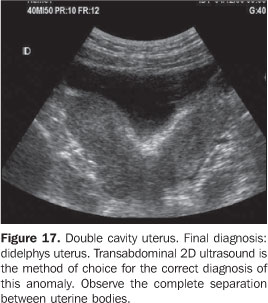
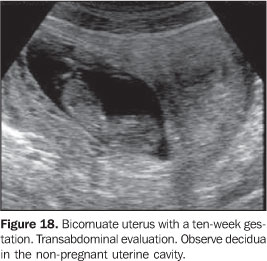
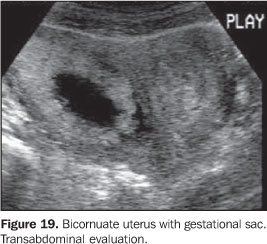
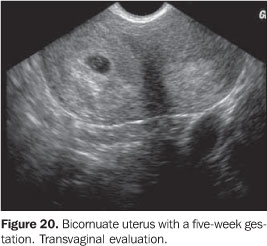
The complete non-fusion of Müllerian ducts originates an anomaly previously called complete double uterus with double cervix, currently denominated didelphys uterus (Figures 16 and 17), with each endometrial cavity ending in a solitary fallopian tube. Such anomalies are perfectly compatible both with normal fertility and menstrual cycles, but sometimes they may result in significant clinical problems(20). Pregnancy in a half of a septate, bicornuate (Figures 18, 19 and 20) or didelphys uterus may be associated with bleeding of the non-pregnant half of the uterus. In rare cases, the pregnancy may occur in a half of the uterus after the other is already pregnant; this is called superfetation. The 2D ultrasound is sufficient for an adequate evaluation and diagnosis.
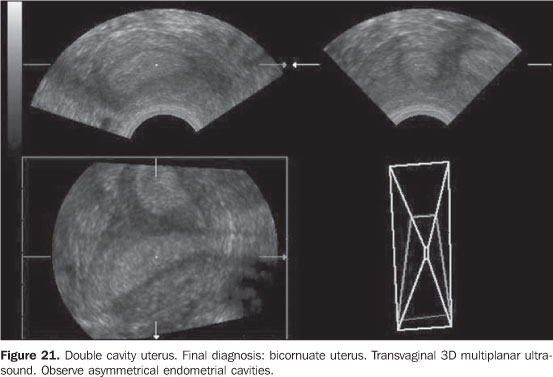
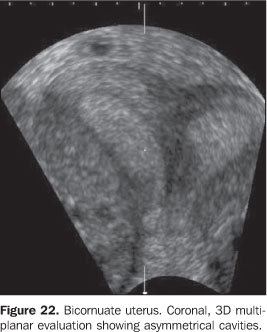
Bicornuate uteri (Figures 21 and 22) is the result of an incomplete fusion of the uterovaginal horns at the level of the fundus; that is to say, a partial fusion has occurred, resulting in two uterine fundi (horns) presenting different fusion degrees, symmetrically or not, most often at the level of the uterine isthmus, and, therefore, frequently presenting a single cervix. This type of anomaly may be confused with septate uterus so currently 3D ultrasound is a valuable diagnostic method.
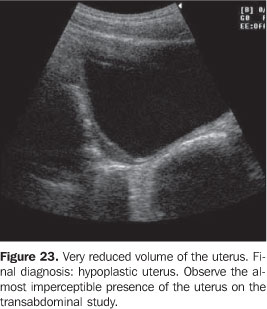
The small sized uterus is subdivided into hypoplastic and infantile uterus. The uterine hypoplasia (Figure 23) is found in an array of endocrine disorders, with a 1:1 uterine body/cervix ratio. In the infantile uterus, the uterine body/cervix ratio is 2:1. In the majority of cases, hypoplastic/infantile uterus occurs because of an ovarian or hypophyseal hypofunction.
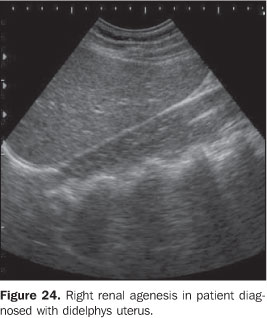
An aspect that should not be disregarded during an ultrasound examination in a patient with uterine malformation is the evaluation of the renal lodges, considering the frequent association of uterine anomalies with urinary tract malformations such as renal agenesis (Figure 24) and/or ectopia(23). Li et al. have found renal agenesis in 17 (29.8%) of 57 patients. No other renal anomaly has been found. Renal agenesis was the most frequent association in patients with didelphys uterus (13/16 cases), uterine agenesis (2/5 cases) and unicornuate uterus (2/7 cases). All the 11 cases of obstructed didelphys uterus were associated with homolateral renal agenesis towards the transverse septum of the obstructed hemivagina. So, they have concluded that renal agenesis is more frequently found in didelphys uterus than in other types of uterine malformations(23).
The uterus and vagina agenesis is denominatedMayer-Rokitansky-Kuster-Hauser syndrome and results fromdysplasia of the Müllerian ducts, with absence of the normaluterus and part or the whole vagina. The diagnosis is basicallyclinical, however, the 2D ultrasound may confirm a clinicalsuspicion. The 3D ultrasound presents no advantage over the 2Dultrasound in these cases. Although there are several types of uterine malformations,almost all of them can be diagnosed as follows: arcuate uterus,septate uterus (partial or complete), bicornuate uterus,unicornuate uterus, didelphys uterus, agenesis, hypoplasia, andinfantile uterus. With the exception of arcuate uterus, considered as a variantof the normal uterus, the most usual uterine anomalies,frequently resulting in diagnostic difficulty are the septate andbicornuate uterus(9). The term "arcuate" refers to cases where there is a minimalalteration of the uterine cavity, with a convex or flat uterinefundus. The endometrial cavity may present a minimal, residualseptum in the fundal region. There is no need for correction. Regardless the type of uterine malformation, both 2D and 3D ultrasound should be performed during the second phase of the menstrual cycle for a better visualization of the endometrium, and therefore a better definition of the uterine cavity. During the first phase of the menstrual cycle, the endometrial cavity may not be appropriately visualized, affecting the diagnosis. In the suspicion of uterine malformations, the evaluation should be always performed during the secretory phase (Figure 5). Alternatively, if this is not feasible, sonohysterography is recommended. Presently, both modalities of 3D ultrasound — multiplanarand volumetric — have been considered as a highly sensitiveand specific technique for uterine malformationsevaluation(24–26). Both the transabdominal andtransvaginal approaches may be adopted, the latest beingpreferable. The transrectal modality is an excellent alternativein the unfeasibility of the transvaginal approach. With themultiplanar 3D ultrasound, longitudinal, axial and coronal planescan be concomitantly evaluated, the coronal plane beingindispensable to an appropriate diagnosis of Müllerian ductsanomalies. Although magnetic resonance imaging is considered by someauthors(12) as the method of choice for uterineanomalies evaluation, with up to 100% efficacy, this has not beena routine practice because of its high cost. For the majority of authors, the ultrasound is the primarymethod for evaluation of Müllerian abnormalities. Fedele etal., studying 43 infertile patients diagnosed with double uterusby hysterosalpingography, have submitted them to subsequentultrasound and laparoscopy/hysteroscopy to evaluate theultrasound capacity to correctly demonstrate a malformed uterus.The ultrasound visualization was adequate in 39 cases (90.7%):one of two cases of didelphys uteri, all the 11 bicornuate uteri,all the four complete septate uteri, and all the 22 partialseptate uteri with 92.3% sensitivity, and 100% specificity.Therefore, a differential and accurate diagnosis of "doubleuterus or endometrial cavity" is possible with thistechnique(21). New diagnostic methods have been introduced, and ultrasoundhas consolidated its position as an invaluable tool to complementthe clinical rationale. Its role in the evaluation of uterinemalformations is already defined and will be more and moreconsolidated with the utilization of the 3D technique.
REFERENCES 1. Ben-Rafael Z, Seidman DS, Recabi K, Bider D, Mashiach S. Uterine anomalies. A retrospective, matched-control study. J Reprod Med 1991;36: 723–727. [ ] 2. Bracci M, Busilacchi P, Ciccognani G, Lorenzoni A, Serri L. Abnormalities of the female genital tract. Comparison of radiographic and echographic pictures. Radiol Med (Torino) 1988;75:181–191. [ ] 3. Matheus M, Franceschini AS, Sala MA, Barrionovo N. Histerossalpingografia: estudo retrospectivo de 535 casos. J Bras Ginecol 1986;96:123–127. [ ] 4. Goldberg JM, Falcone T, Attaran M. Sonohysterographic evaluation of uterine abnormalities noted on hysterosalpingography. Hum Reprod 1997;12: 2151–2153. [ ] 5. De Meo I. Hysterosalpingography in the diagnosis of uterine malformations. Minerva Ginecol 1983;35:127–130. [ ] 6. Valli E, Zupi E, Marconi D, et al. Hysteroscopic findings in 344 women with recurrent spontaneous abortion. J Am Assoc Gynecol Laparosc 2001;8:398–401. [ ] 7. Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update 2001;7:161–174. [ ] 8. Jurkovic D, Gruboeck K, Tailor A, Nicolaides KH. Ultrasound screening for congenital uterine anomalies. Br J Obstet Gynaecol 1997;104:1320–1321. [ ] 9. Raga F, Bonilla-Musoles F, Blanes J, Osborne NG. Congenital mullerian anomalies: diagnostic accuracy of three-dimensional ultrasound. Fertil Steril 1996;65:523–528. [ ] 10. Chan L, Uerpairojkit B, Reece EA. Diagnosis of congenital malformations using two-dimensional and three-dimensional ultrasonography. Obstet Gynecol Clin North Am 1997;24:49–69. [ ] 11. Lev-Toaff AS, Pinheiro LW, Bega G, Kurtz AB, Goldberg BB. Three-dimensional multiplanar sonohysterography: comparison with conventional two-dimensional sonohysterography and x-ray hysterosalpingography. J Ultrasound Med 2001;20:295–306. [ ] 12. Fedele L, Dorta M, Brioschi D, Massari C, Candiani GB. Magnetic resonance evaluation of double uteri. Obstet Gynecol 1989;74:844–847. [ ] 13. Propst AM, Hill JA 3rd. Anatomic factors associated with recurrent pregnancy loss. Semin Reprod Med 2000;18:341–350. [ ] 14. Nouira M, Slama A, Essaidi H, et al. Pregnancy in the malformed uterus. Study of 366 pregnancies. Tunis Med 1998;76:376–379. [ ] 15. Ramos LO, Motta EV. Malformações genitais sem conotação com intersexo. In: Tratado de ginecologia Febrasgo. 1ª ed. Rio de Janeiro: Revinter, 2000;375–386. [ ] 16. Ayida G, Kennedy S, Barlow D, Chamberlain P. Contrast sonography for uterine cavity assessment: a comparison of conventional two-dimensional with three-dimensional transvaginal ultrasound; a pilot study. Fertil Steril 1996;66:848–850. [ ] 17. Jones Jr HW . Reproductive impairment and the malformed uterus. Fertil Steril 1981;36:137–148. [ ] 18. Nicolini U, Bellotti M, Bonazzi B, Zamberletti D, Candiani GB. Can ultrasound be used to screen uterine malformations? Fertil Steril 1987;47:89–93. [ ] 19. Woodward PJ, Sohaey R, Wagner BJ. Congenital uterine malformations. Curr Probl Diagn Radiol 1995;24:178–197. [ ] 20. Heinonen PK, Savolainen A, Pystynen P. Septate uterus and habitual abortion: a case report illustrating successful outcome of pregnancy after second metroplasty. Eur J Obstet Gynecol Reprod Biol 1986;23:233–238. [ ] 21. Fedele L, Ferrazzi E, Dorta M, Vercellini P, Candiani GB. Ultrasonography in the differential diagnosis of "double" uteri. Fertil Steril 1988;50: 361–364. [ ] 22. Woelfer B, Salim R, Banerjee S, Elson J, Regan L, Jurkovic D. Reproductive outcomes in women with congenital uterine anomalies detected by three-dimensional ultrasound screening. Obstet Gynecol 2001;98:1099–1103. [ ] 23. Li S, Qayyum A, Coakley FV, Hricak H. Association of renal agenesis and mullerian duct anomalies. J Comput Assist Tomogr 2000;24:829–834. [ ] 24. Wu MH, Hsu CC, Huang KE. Detection of congenital mullerian duct anomalies using three-dimensional ultrasound. J Clin Ultrasound 1997; 25:487–892. [ ] 25. Hosli IM, Tercanli S, Herman A, Kretschmann M, Holzgreve W. In vitro volume measurement by three-dimensional ultrasound: comparison of two different systems. Ultrasound Obstet Gynecol 1998;11:17–22. [ ] 26. Balen FG, Allen CM, Gardener JE, Siddle NC, Lees WR. 3-dimensional reconstruction of ultrasound images of the uterine cavity. Br J Radiol 1993;66:588–591. [ ]
Received December 20, 2004.
* Study developed at EURP – Escola de Ultra-sonografia e Reciclagem Médica de Ribeirão Preto, Ribeirão Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554