INTRODUCTION
Short bowel syndrome (SBS) occurs when there is a reduction of the functional mass of the small bowel, leading to nutritional deficit(1,2). In adults, 75% of the SBS cases originate from massive intestinal resections related to mesenteric infarction, small bowel volvulus, traumatic injury to superior mesenteric vessels and adherences(3). Multiple intestinal resections because of Crohn’s disease and actinic enteritis correspond to 25% of SBS cases. The reduction in the absorptive surface and the increase in intestinal transit velocity lead to profuse diarrhea, dehydration, changes in the electrolyte balance and acid-alkaline balance, in addition to nutritional impairment(4).
In healthy individuals, the small bowel length ranges between 300 and 850 cm, with the proximal two fifths represented by the jejunum, and the remainder, by the ileum. Intestinal resection is considered small when the remaining bowel is 100 to 150 cm long. Large resections are those in which the remaining bowel is between 40 and 100 cm long; and massive resections are those in which the remnants of the bowel are less than 40 cm long(5). Small bowel syndrome may be characterized according to the intestinal segment that has been removed, as follows:
a) predominantly jejunal resection, with distal ileum longer than 10 cm and preservation of the ileocecal valve and all the colonic segments;
b) ileal resection with preservation of the ileocecal valve;
c) Ileal and ileocecal valve resection with jejunocolonic anastomosis;
d) partial jejunal resection and total ileocolonic resection with terminal jejunostomy.
The progression tends to be satisfactory when the resections are smaller than 80% of the total length of the bowel. The ileum has a greater adaptive capacity, which implies a better prognosis after jejunal resection than in the event of ileal resection(6). The preservation of the ileocecal valve may slow down the intestinal transit time and prevent reflux of the colonic content into the small bowel. The colon preservation maintains the hydric absorption, avoiding watery diarrhea and dehydration, besides slowing down the intestinal transit and stimulating hyperplasia of the small bowel.
After three to 12 months from resection, adaptive changes occur in the remnant bowel, in the attempt to compensate the reduction of the absorptive surface. The factors involved in the intestinal adaptation include the length, topography and conditions of the remaining segment, the patient’s age and nutritional therapeutics adopted, with emphasis on the oral approach(7).
The objective of the present essay is to demonstrate the contribution of the study of intestinal transit in the initial assessment and follow-up of patients with SBS, with emphasis on the radiographic aspects of structural changes arising from the intestinal adaptation. With a view on such purpose, the authors selected illustrative confirmed cases of SBS assisted in their institution from 2000 to 2010.
INTESTINAL TRANSIT IN THE ASSESSMENT OF SBS PATIENTS
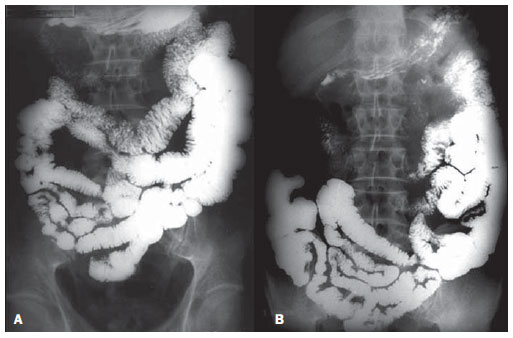
Figure 1 exemplifies the normal intestinal transit, for comparative illustration with Figures 2, 3, 4A and 4B, which depict contrast-enhanced examinations of SBS patients.
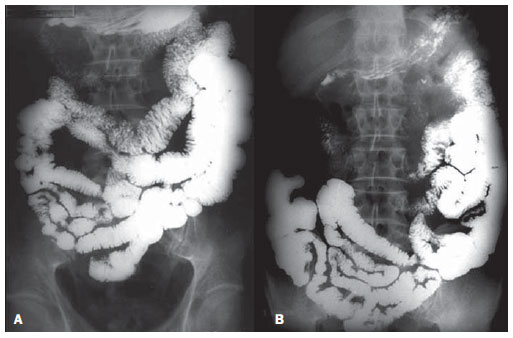
Figure 1. Normal intestinal transit. A: presence of contrast in jejunal and ileal loops with one hour of observation. B: Arrival of the contrast agent at the terminal ileum and cecum, at two hours of intestinal transit.
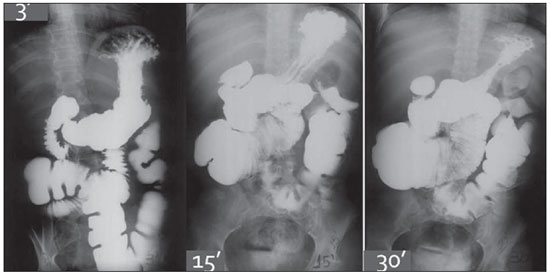
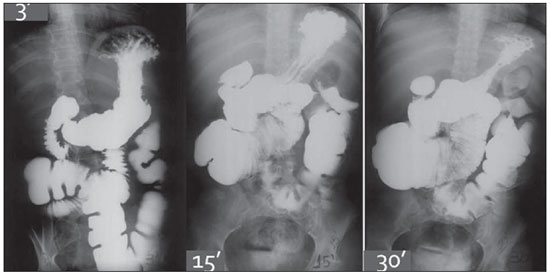
Figure 2. Intestinal transit time test in a SBS patient. Arrival of the contrast agent at the transverse colon, at three minutes of the study.
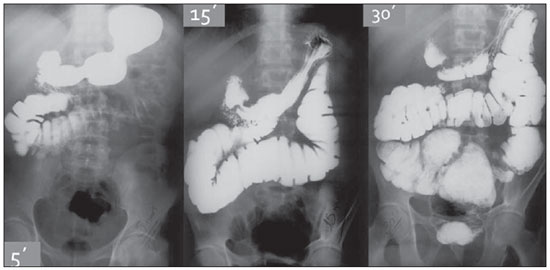
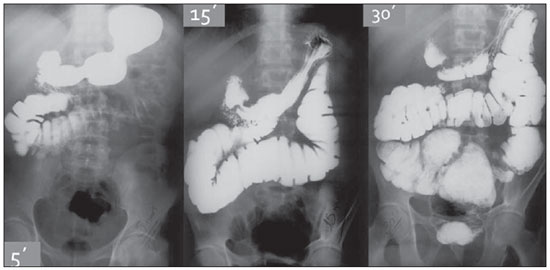
Figure 3. SBS patient. Filling of the rectal ampulla by the contrast agent is observed at 30 minutes of study.
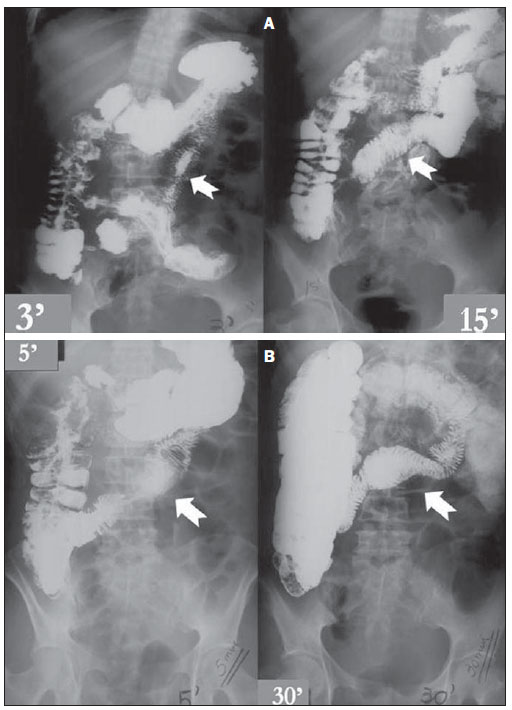
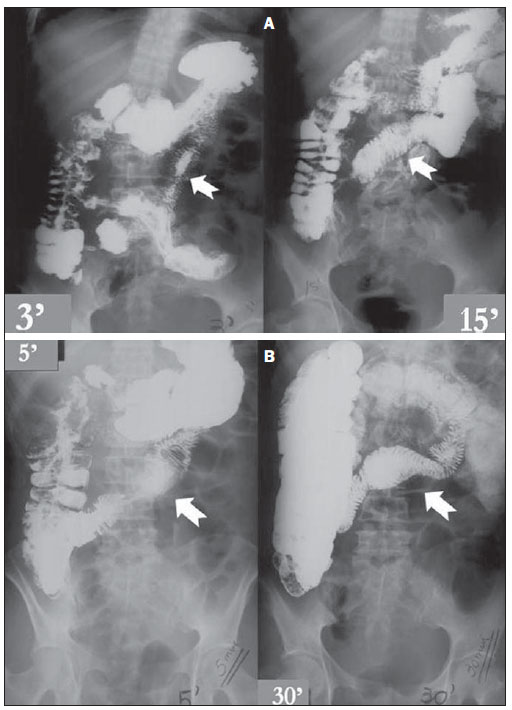
Figure 4. A: Intestinal transit time test in a SBS patient, completing the intestinal transit in three minutes. Note the appearance of small mucosal folds (arrows) and compare them with Figure 4B. B: Intestinal transit time test in the same patient on Figure 4A, after three years, demonstrating findings of intestinal structural adaptation, with increased mucosal folding and dilation in small bowel loops.
On Figure 2, the intestinal transit study of a 37-year-old female patient is observed. The patient had undergone massive enterectomy due to entero-mesenteric infarction, with surgical jejunocolonic anastomosis (transverse colon) and presence of 15 cm of remnant small bowel. The presence of contrast is observed within the colonic loops at 3 minutes of the study. Also, the increased caliber of the remnants of the small bowel loops and hypertrophy of the mucosal folds are observed, characterizing the ongoing intestinal adaptation.
On Figure 3, another example of intestinal transit in a SBS patient with history of mesenteric ischemia. Male 48-year-old patient submitted to massive intestinal resection that left 15 cm of remnant functional bowel. Note that there is almost a direct passage of contrast from the duodenum to the colonic loops, with a minimal length of interposed small bowel, and filling of the rectal ampulla by the contrast medium at 30 minutes of study, characterizing extremely fast intestinal and colonic transit, with reserved prognosis, restricting the possibilities of nutritional therapies.
Figures 4A and 4B illustrate the case of a female 49-year-old patient who had an entero-mesenteric infarction, submitted to massive resection of the small bowel, with only 20 cm of functional bowel being left. The images were obtained in the patient follow-up, with an elapsed time of three years between both images. Figure 4B shows is the most recent image. In this example, it is observed that, in spite of no significant change in the intestinal transit time between the studies, it is clear that, on the images on Figure 4B, after three years of progression, the patient presented a significant increase in mucosal folding and focal dilation of certain intestinal segments. Such changes leave no doubts on the existence and magnitude of the intestinal adaptation phenomenon and its potential for improving the nutritional prognosis of such patients.
DISCUSSION
The selection of the most appropriate method for the diagnosis of intestinal disorders must be based on clinical observations and on the availability of the different methods at the center. Except for the proximal segments of the jejunum (which occasionally may be evaluated by means of upper endoscopy) and the terminal ileum (which can be approached by colonoscopy), the largest part of the small bowel can only be evaluated by imaging methods. In spite of the availability of modern imaging methods, contrast-enhanced intestinal transit study still continues to be a reference method for the detection of intraluminal morphological changes in the small bowel(8,9).
Intestinal transit time test is a relatively simple and widely available study, with few contraindications or associated complications. Additionally, such study provides complete and detailed information on the small bowel, such as shape, contours, distribution of intestinal loops, characteristics of the mucosal surface pattern, motility and intestinal transit time.
The findings of radiographic images of SBS patients described on the present essay, allowed the evaluation of the remnant bowel length, the characterization and stratification of intestinal structural adaptations and motility by measuring the intestinal transit time. The length of the small bowel observed on the intestinal transit study is correlated with the measurements performed during the surgical procedure, and are clinically significant for the definition of the prognosis and of the appropriate approach for nutritional therapy administration.
The barium follow through series demonstrated adaptive changes in the remnant intestinal segments, expressed by mucosal folds hypertrophy and by the increased caliber of the intestinal loops. Such findings are compatible with histological changes observed after intestinal resections, characterized by hyperplasia of the villous cells, increased crypts depth, mucosal hyperplasia and dilation of the remnant segment, which implies a larger absorptive surface(10).
The findings described at the intestinal transit test for SBS may also be easily observed at CT enterography and MRI enterography. Eventually, such imaging methods may be utilized, particularly in cases where complications such as intestinal obstruction, abdominal collections and mesenteric vascular abnormalities are suspected.
CONCLUSIONS
SBS is a complex clinical condition, which requires an interdisciplinary approach with a view on the most physiological and appropriate nutritional therapy to suit individual needs. The present essay demonstrates the essentiality of barium follow through in the initial evaluation as well as in the periodic follow-up of SBS patients. Such method allows the structural and dynamic evaluation of the remnant bowel, documenting the adaptive phenomena which drastically interfere with the clinical progression of SBS patients.
REFERENCES
1. Donohoe CL, Reynolds JV. Short bowel syndrome. Surgeon. 2010;8:270—9.
2. Keller J, Panter H, Layer P. Management of short bowel syndrome after extensive small bowel resection. Best Pract Res Clin Gastroenterol. 2004;18:977—92.
3. Broadbent AM, Heaney A, Weyman K. A review of short bowel syndrome and palliation: a case report and medication guideline. J Palliat Med. 2006;9:1481—91.
4. Thompson JS, DiBaise JK, Iyer KR, et al. Postoperative short bowel syndrome. J Am Coll Surg. 2005;201:85—9.
5. Goday PS. Short bowel syndrome: how short is too short? Clin Perinatol. 2009;36:101—10.
6. Yamataka A, Kato Y. Long-term outcome of short bowel syndrome. Nippon Geka Gakkai Zasshi. 2009;110:199—202.
7. Marchini JS, Unamuno MRDL, Carneiro JJ, et al. Três anos de experiência e seguimento de pacientes portadores de síndrome do intestino curto e/ou síndrome de má absorção grave, portadores de desnutrição refratária a dietoterapia via oral (DRD). Rev Bras Nutr Clin. 1996;11:27—34.
8. Joly F, Mayeur C, Messing B, et al. Morphological adaptation with preserved proliferation/transporter content in the colon of patients with short bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2009;297:G116—23.
9. Levine MS, Rubesin SE, Laufer I. Pattern approach for diseases of mesenteric small bowel on barium studies. Radiology. 2008;249:445—60.
10. D’Eredità G, Ferrarese F, Cecere V, et al. Factors affecting prognosis in patients with short bowel syndrome. G Chir. 2003;24:302—4.
1. MDs, Residents at the Division of Radiology, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
2. PhDs, Professors at Division of Radiology, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
3. Titular Professor in the Division of Nutrology, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
4. PhD, Professor, Division of Nutrology, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
Mailing Address:
Dr. Francisco Abaeté das Chagas Neto
Secretaria do Setor de Radiologia (CCIFM), Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo
Avenida Bandeirantes, 3900, Campus Universitário, Monte Alegre
Ribeirão Preto, SP, Brazil, 14048-900
E-mail: abaeteneto@yahoo.com.br
Received October 17, 2010.
Accepted after revision March 15, 2011.
Study developed at Centro de Ciências das Imagens e Física Médica (CCIFM) do Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil.
 Vol. 44 nº 3 - May / June of 2011
Vol. 44 nº 3 - May / June of 2011