Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 1 - Jan. /Feb. of 2012
Vol. 45 nº 1 - Jan. /Feb. of 2012
|
CASE REPORT
|
|
Can pregnancy influence the outcome of a malignant thyroid nodule? |
|
|
Autho(rs): Lucy Kerr1; Maria Edith Lutz Vidigal2; Deborah Rozenkwit3 |
|
|
Keywords: Pregnancy; Cancer; Thyroid; Carcinoma; Papillary. |
|
|
Abstract: INTRODUCTION
It has been reported that thyroid cancer worsens during pregnancy(1—3) and the worst prognosis would be related to the estrogen receptor alpha-mediated growth factor, whose expression is enhanced in thyroid tumors that run their courses with pregnancy(1). The present case report describes a thyroid nodule followed-up before, during pregnancy and during lactation, that had presented a 58% decrease in volume since its diagnosis with benign sonographic and cytopathological features(4). Sonographic findings suggesting malignancy only were detected during pregnancy and lactation, when fine-needle aspiration puncture (FNAP) was repeated, demonstrating the presence of a papillary carcinoma. In the present case, the follow-up of the disease progression was critical for the detection of the change in the morphological texture and Doppler patterns, suggesting the lesion malignancy and allowing the adoption of an appropriate approach. CASE REPORT A female 31-year-old patient accidentally detected a thyroid nodule, whose first FNAP performed on August 9, 2005 diagnosed a benign hemorrhagic cystic lesion. On November 3, 2005, ultrasonography (US) demonstrated the presence of a mass with mixed echogenicity in the left thyroid lobe (Figure 1), with a benign pattern, and measuring 1.2 × 0.8 × 0.6 cm in the longitudinal, transverse and anteroposterior diameters, respectively, and whose cystic component presented fluid-fluid level suggesting density stratification like in the mixture of water and oil, that is frequently found in cases of intranodular hemorrhage. Doppler study demonstrated a single vessel penetrating the vegetation (Figure 2). A further US study performed on October 6, 2006 revealed a 33% decrease in the nodular volume resulting from partial fluid resorption, while the solid component of the mass remained unchanged. On November 4, 2009, at the 22nd week of pregnancy, US study (Figure 3) revealed a 36% nodule volume decrease resulting from cystic resorption, since the vegetation had tripled in volume and presented hypervascularization, both signs suspicious for malignancy(1,4,5). A second US-guided FNAP was indicated and performed on April 23, 2010, suggesting two hypotheses: pseudo-papilliferous hyperplasia in adenomatous goiter, or papillary carcinoma. Another sonographic study performed on May 10, 2010, 40 days after delivery, demonstrated that the thyroid nodule had grown 2.3 times in six months, was totally solid, poorly delimited, hypoechogenic and presented microcalcifications, suggesting malignancy(4) (Figure 4). Surgery was performed on May 20, 2010, with diagnosis of a classical pattern of a T1A stage encapsulated papillary carcinoma measuring 0.5 cm.  Figure 1. First ultrasonography study (November 3, 2005) demonstrating a mixed nodule in the left thyroid lobe, with benign morphologic pattern and with cystic component presenting density stratification like in water and oil mixture, that is a frequent finding in intranodular hemorrhage. 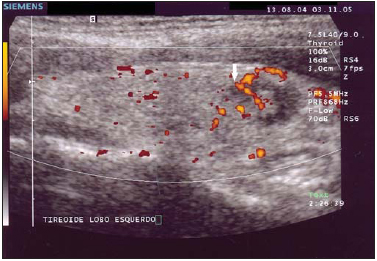 Figure 2. Doppler study of the nodule in the left thyroid lobe showing a vessel penetrating the vegetation (arrow), characterizing it is as live tissue (blood clot is excluded). 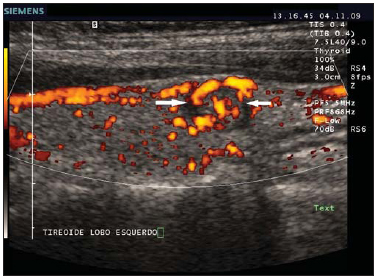 Figure 3. Twenty-second week of gestation. Longitudinal section of a nodule in left thyroid lobe with hypervascularization in the solid component (arrows). 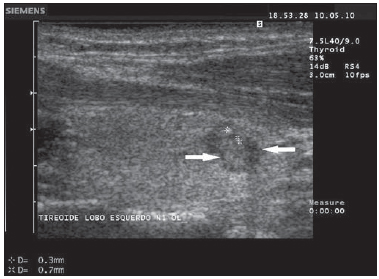 Figure 4. Forty days after delivery, the nodule in the left thyroid lobe (arrows) is completely solid, poorly delimitated, hypoechogenic and with microcalcifications (calipers). DISCUSSION The initial FNAP and US classified the lesion as a benign thyroid nodule, but it was malignant when it was operated three years after the diagnosis. Although the presence of a single vessel in the central region of the mass at the initial Doppler study is considered as a suspicious sign of malignancy by some authors(6,7), others only consider the Doppler pattern as malignant in cases where de mass is completely hypervascularized(4,5,8), and the 2008 consensus indicates FNAP for the investigation of such nodules(5). Two hypotheses prevail in the present case: either the nodule was benign and became malignant, or it was already malignant (false-negative at FNAP and US), accelerating its growth during pregnancy. It was observed that the nodule decreased about 58% between the first and the third US studies, the fluid component was resorpted, and suspicious signs appeared: a three-fold increase in size and hypervascularization of the solid component. It is more likely that malignancy was present since the beginning, and the pregnancy contributed to the accelerated growth of the mass. The US follow-up allowed the investigators to raise the suspicion of malignancy that was confirmed by FNAP. The authors conclude that the pregnancy may have influenced the growth of the pre-existing malignant thyroid nodule, and that the evolutive follow-up was fundamental to the correct diagnosis in the present case. REFERENCES 1. Vannucchi G, Perrino M, Rossi S, et al. Clinical and molecular features of differentiated thyroid cancer diagnosed during pregnancy. Eur J Endocrinol. 2010;162:145—51. 2. Vini L, Hyer S, Pratt B, et al. Management of differentiated thyroid cancer diagnosed during pregnancy. Eur J Endocrinol. 1999;140:404—6. 3. Wémeau JL, Do Cao C. Thyroid nodule, cancer and pregnancy. Ann Endocrinol (Paris). 2002;63:438—42. 4. Kerr L. High-resolution thyroid ultrasound: the value of color Doppler. Ultrasound Q. 1994;12:21—43. 5. Cibas ES, Alexander EK, Benson CB, et al. Indications for thyroid FNA and pre-FNA requirements: a synopsis of the National Cancer Institute Thyroid Fine-Needle Aspiration State of the Science Conference. Diagn Cytopathol. 2008;36:390—9. 6. Chammas MC, Gerhard R, Oliveira IRS, et al. Thyroid nodules: evaluation with power Doppler and duplex Doppler ultrasound. Otolaryngol Head Neck Surg. 2005;132:874—82. 7. Lagalla R, Caruso G, Novara V, et al. Analisi flussimetrica nella patologia tiroidea: ipotesi di integrazione con lo studio qualitativo con color-Doppler. Radiol Med. 1993;85:606—10. 8. Faria MAS, Casulari LA. Comparação das classificações dos nódulos de tireoide ao Doppler colorido descritas por Lagalla e Chammas. Arq Bras Endocrinol Metab. 2009;53:811—7. 1. MD, Medical Sonographer, Director, IKEP-Instituto Kerr de Ensino e Pesquisa and Sonimage, São Paulo, SP, Brazil. 2. MD, Endocrinologist, Member of Sociedade Brasileira de Endocrinologia, São Paulo, SP, Brazil. 3. MD, General Clinician, Trainee in Ultrasonography at IKEP-Instituto Kerr de Ensino e Pesquisa, São Paulo, SP, Brazil. Mailing Address: Dra. Lucy Kerr Avenida Brigadeiro Luís Antônio, 2504, 2º andar, conjunto 21/22, Jardim Paulista São Paulo, SP, Brazil, 01402-000 E-mail: lucykerr@lucykerr.com.br Received December 12, 2010. Accepted after revision August 11, 2011. Study developed at IKEP-Instituto Kerr de Ensino e Pesquisa, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554