Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 51 nº 1 - Jan. /Feb. of 2018
Vol. 51 nº 1 - Jan. /Feb. of 2018
|
ORIGINAL ARTICLE
|
|
Computed tomography angiography study of variations of the celiac trunk and hepatic artery in 100 patients |
|
|
Autho(rs): Ivelise Regina Canito Brasil1; Igor Farias de Araujo2; Adriana Augusta Lopes de Araujo Lima3; Ernesto Lima Araujo Melo4; Ronaldo de Matos Esmeraldo5 |
|
|
Keywords: Anatomy; Computed tomography, Celiac artery; Hepatic artery; Liver transplantation. |
|
|
Abstract: INTRODUCTION
The trifurcation of the celiac trunk was first described by Haller in 1756. In 1955, Michels developed a system for classifying the anatomical pattern of the celiac trunk, based on the dissection of 200 cadavers. In 1966, an international classification system for anatomical variations of the hepatic artery was proposed(1–5). The celiac trunk and the superior mesenteric artery are two branches of the abdominal aorta. The celiac trunk emerges from just below the aortic hiatus at the level of the transition from the thoracic vertebrae to the lumbar vertebrae. In the so-called “normal” anatomical pattern, the celiac trunk trifurcates (into the splenic artery, common hepatic artery, and left gastric artery) slightly below the point at which it emerges from the aorta(4,6–11). It is now known that the abdominal vasculature has several common patterns of origin. Knowledge of the most common anatomical variations is crucial in surgical planning and in interventional examinations(6,10,12–19). With advances in the imaging techniques employed in angiography—computed tomography (CT) and magnetic resonance—not only in data acquisition but also in image post-processing on workstations, it is possible to obtain information that facilitates the planning of a given surgical procedure, which can, ultimately, contribute to reducing the associated rates of morbidity and mortality. For example, one important application that requires a detailed knowledge of the vascular anatomy is the infusion of chemotherapy via catheter for the treatment of unresectable malignant liver tumors. Laparoscopic surgery can be understood as a model of the importance of recognizing vascular variations in order to avoid iatrogenic complications, given that the surgical field is limited(11,13,14,16,18–22). As it evolved, CT began to allow the acquisition of a greater quantity of computerized images in a shorter period of time, through the use of scanners with multiple rows of submillimeter detectors. Thus, CT facilitated the acquisition of images of the standard abdominal vasculature and its variations, as an aid in emergency situations, such as gastrointestinal bleeding(11,13,16,18,20,21,23). The objective of the present study was to evaluate the patterns of anatomical variations of the celiac trunk and hepatic artery. To that end, we analyzed CT angiography examinations performed in multidetector scanners. MATERIALS AND METHODS The study was approved by the Research Ethics Committee of the General Hospital of Fortaleza, located in the city of Fortaleza, in the state of Ceará, Brazil. All of the patients included in the study had received a physician referral for the examination, due to causes unrelated to the research, and it was therefore unnecessary to obtain written informed consent. We prospectively analyzed 100 consecutive CT angiography examinations of the abdomen performed at the General Hospital of Fortaleza between June 2013 and June 2014. We excluded patients with a history of abdominal surgery. CT examination The examinations were performed on a 64-channel multislice CT scanner (Brilliance; Philips Healthcare, Eindhoven, The Netherlands). We acquired source images with a thickness of 0.6 mm, reconstructed with a thickness of 2 mm and an increment of 1 mm. The contrast medium used was iobitridol (300 mg/mL, Henetix 300; Guerbet Produtos Radiológicos, Rio de Janeiro, Brazil), which was administered intravenously by injection pump (OptiVantage; Mallinckrodt, Cincinnati, OH, USA), with an 18–20 gauge catheter for peripheral access in the arm, at a flow rate of 4 mL/s. None of the patients included in this study had a reaction to the use of contrast. Radiological interpretation The imaging data obtained were archived electronically and restored on a workstation (Advantage Workstation 4.4; General Electric Healthcare, Milwaukee, WI, USA), after which they were reconstructed by multiplanar reconstruction, maximum intensity projection, and volume rendering. Those techniques were actively applied during the interpretation phase, the images being interpreted by a radiologist with 14 years of experience in abdominal and vascular imaging. In this study, we analyzed the anatomy of the celiac trunk, as well as the origins of the common hepatic, splenic, left gastric, and superior mesenteric arteries. We also examined the origins of the right hepatic artery, the left hepatic artery, the gastroduodenal artery, and any accessory hepatic arteries. RESULTS Variations of the celiac trunk The anatomy of the celiac trunk was categorized according to the classification system devised by Sureka et al.(3), as detailed in Table 1. We identified the normal anatomical pattern—the hepatogastrosplenic trunk and superior mesenteric artery originating from the abdominal aorta—in 43% of the cases. We also identified five patterns of anatomical variations: a hepatosplenic trunk with the left gastric artery emerging 0.4–2.5 cm above the bifurcation of the celiac trunk and the superior mesenteric artery emerging from the abdominal aorta, in 47% of the cases; a gastrosplenic trunk with the common hepatic artery and superior mesenteric artery originating from the abdominal aorta, in 2%; a gastrosplenic trunk with the hepatic artery emerging from the superior mesenteric artery, in 3%; a hepatosplenic mesenteric trunk with the left gastric artery originating from the abdominal aorta, in 1%; and an ambiguous anatomical pattern, which did not meet the criteria for any of the other patterns, in 4%. 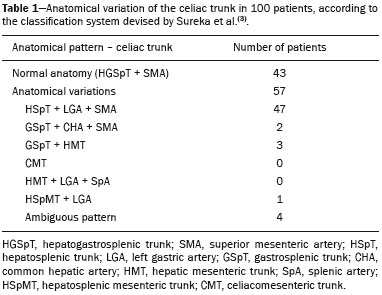 Variations of the hepatic artery The anatomy of the hepatic artery was categorized according to the classification system devised by Michels(5), as detailed in Table 2. We identified the normal anatomical pattern—the hepatic artery emerging from the common hepatic artery and bifurcating into the right and left hepatic arteries, designated type I—in 82% of the cases. We also identified six patterns of anatomical variations: the left hepatic artery emerging from the left gastric artery (type II), as illustrated in Figure 1, in 1% of the cases; the right hepatic artery emerging from the superior mesenteric artery (type III), in 10%; an accessory left hepatic artery emerging from the left gastric artery (type V), in 1%; an accessory right hepatic artery emerging from the superior mesenteric artery (type VI), in 1%; a common hepatic artery emerging from the superior mesenteric artery (type IX), as illustrated in Figure 2, in 4%; and an unspecified anatomical pattern (type XI), in 1%. None of the patients in our study showed the Michels type IV, VII, VIII, or X anatomical pattern. 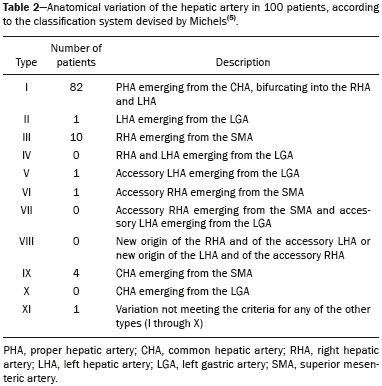  Figure 1. CT angiography reconstruction by maximum intensity projection showing the left hepatic artery (arrowhead) emerging from the left gastric artery.  Figure 2. CT angiography reconstruction by maximum intensity projection in the coronal plane, showing the common hepatic artery (arrowhead) emerging from the superior mesenteric artery (arrow). DISCUSSION We prospectively analyzed 100 consecutive CT angiography examinations of the abdomen performed at the General Hospital of Fortaleza over a one-year period. The imaging evaluation of the rhino-orbital region has been the object of a series of recent publications in the radiology literature of Brazil(24–29). In the standard definition of the visceral anatomy, the celiac trunk originates from the abdominal aorta and trifurcates into the left gastric artery, splenic artery, and common hepatic artery(4,7,30). Although there are 15 possible patterns of anatomical variations of the celiac trunk, we detected, in our study, only six types, the same number found in the study conducted by Sureka et al.(3). In our study, the normal anatomic pattern of the celiac trunk was found in 43% of the cases, compared with 89% in the dissection study conducted by Michels(5); 91% in the study conducted by Sureka et al.(3); 86% in the study conducted by Sankar et al.(8); 85.1%, 89.5%, and 95.4%, respectively, in cadaver studies, imaging studies, and liver transplantation studies, as reported by Panagouli et al.(31); 89.1% in the study conducted by Song et al.(18); 89.8% in the study conducted by Chen et al.(32), who analyzed a population defined as homogeneous in Japan; and 90% in the study conducted by Araujo-Neto et al.(33). We identified variations of the celiac trunk in 57% of the patients in our sample, compared with the 10.6% reported by Panagouli et al.(31), the 5.5% reported by Sureka et al.(3), the 14% reported by Sankar et al.(8), the 9.6% reported by Song et al.(18) , and the 10.2% reported by Chen et al.(32). The most common anatomical pattern of variation in our study—found in 47% of the cases—was a hepatosplenic trunk with the left gastric artery emerging 0.4–2.5cm above the bifurcation of the celiac trunk and the superior mesenteric artery originating from the abdominal aorta. That anatomical pattern was also observed by Sureka et al.(3), Michels(5), and Song et al.(18) , although in only 2.3%, 4%, and 4.42% of the cases, respectively. In the study conducted by Araujo-Neto et al.(33), the most common anatomical pattern of variation—found in 8.3% of the cases—was a hepatosplenic trunk with the left gastric artery originating from the abdominal aorta. Regarding the anatomy of the hepatic artery, the most commonly seen pattern, according to the classification system devised by Michels(5), is type I; that is, the hepatic artery emerging from the common hepatic artery and bifurcating into the right and left hepatic arteries(5). In our study, we found Michels type I anatomical pattern of the hepatic artery in 82% of the cases, whereas Gumus et al.(15), Sureka et al.(3), and Chen et al.(1) reported Michels type I anatomical pattern in 66.8%, 55%, and 51%, respectively. In a cadaver study conducted in Brazil, Sebben et al.(2) identified Michels type I anatomical pattern in 73% of the cadavers dissected. In a liver transplantation study conducted in the Brazilian state of Paraná, Freitas et al.(30) found the normal anatomical pattern in 76.82% of the cases. In our study, 18% of the patients had some variation in the anatomy of the hepatic artery, compared with 33.2% reported by Gumus et al.(15), 45% reported by Sureka et al.(3), 49% reported by Chen et al.(1), 27% reported by Sebben et al.(2), 23.18% reported by Freitas et al.(30), 10.2% reported by Chen et al.(32), and 21.7% reported by Araujo-Neto et al.(33). The most common anatomical pattern of variation in our study—found in 10% of the cases—was the right hepatic artery emerging from the superior mesenteric artery. In the studies analyzed, that was also the main pattern of anatomical variation, although in different proportions of the samples evaluated. Gumus et al.(15), reported that same pattern in 10.1% of the patients in their sample, comparable to the 11% reported by Sureka et al.(3), the 15% reported by Chen et al.(1), the 10% reported by Sebben et al.(2), and the 11.38% reported by Freitas et al.(30). Our study provides an insight into the anatomical patterns found in Brazil. In view of our findings, it is possible to conclude that, because of the extensive miscegenation in Brazil, the indices of anatomical variation, despite sharing points of similarity, also present patterns of variations that differ considerably from those reported in the international literature, especially when we compare the patterns of celiac trunk variation with those found in homogeneous populations(2,9,14,32). It is noteworthy that some isolated studies conducted in Brazil have analyzed the anatomical pattern of the hepatic artery and its branches in cadavers and during liver transplantations. However, studies dealing with the anatomical variations of the celiac trunk are really quite rare in Brazil, this being the aspect of our study that distinguishes it from others in the literature(2,9,14,22,30). On the basis of our findings, we can state that studies like ours are scarce and should be encouraged, in order to improve understanding of the anatomical patterns in the population of Brazil. Further studies of this nature could lead to better technical planning of surgical procedures and could avoid inadvertent injuries that might compromise the results of medical procedures, leading to complications. Better knowledge of anatomical variations could ultimately contribute to reducing the rates of morbidity and mortality in endovascular procedures, abdominal surgeries, and transplantations, especially those of the liver and pancreas(2,14,22,30). REFERENCES 1. Chen H, Yano R, Emura S, et al. Anatomic variation of the celiac trunk with special reference to hepatic artery patterns. Ann Anat. 2009;191:399–407. 2. Sebben GA, Rocha SL, Sebben MA, et al. Variações da artéria hepática: estudo anatômico em cadáveres. Rev Col Bras Cir. 2012; 40:221–6. 3. Sureka B, Mittal MK, Mittal A, et al. Variations of celiac axis, common hepatic artery and its branches in 600 patients. Indian J Radiol Imaging. 2013;23:223–33. 4. Venieratos D, Panagouli E, Lolis E, et al. A morphometric study of the celiac trunk and review of the literature. Clin Anat. 2013; 26:741–50. 5. Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966;112:337–47. 6. Catalano OA, Singh AH, Uppot RN, et al. Vascular and biliary variants in the liver: implications for liver surgery. Radiographics. 2008;28:359–78. 7. Nayak SR, Prabhu LV, Krishnamurthy A, et al. Additional branches of celiac trunk and its clinical significance. Rom J Morphol Embryol. 2008;49:247–9. 8. Sankar KD, Bhanu PS, Susan PJ. Variant anatomy of the celiac trunk and its branches. Int J Morphol. 2011;29:581–4. 9. Varma KS, Pamidi N, Vollala VR. Common celiacomesenteric trunk: a rare anatomic variation. J Vasc Bras. 2009;8:271–3. 10. Wang Y, Cheng C, Wang L, et al. Anatomical variations in the origins of the celiac axis and the superior mesenteric artery: MDCT angiographic findings and their probable embryological mechanisms. Eur Radiol. 2014;24:1777–84. 11. Melo-Leite AF, Mota Jr A, Chagas-Neto FA, et al. Acquired portosystemic collaterals: anatomy and imaging. Radiol Bras. 2016;49:251–6. 12. Atasoy Ç, Ozyürek E. Prevalence and types of main and right portal vein branching variations on MDCT. AJR Am J Roentgenol. 2006; 187:676–81. 13. Winston CB, Lee NA, Jarnagin WR, et al. CT angiography for delineation of celiac and superior mesenteric artery variants in patients undergoing hepatobiliary and pancreatic surgery. AJR Am J Roentgenol. 2007;188:W13–9. 14. Freitas ACT, Godoy JL, Matias JEF, et al. Comparação entre exames de imagem e achados operatórios em doadores para transplante hepático intervivos. Arq. Gastroenterol. 2007;44:325–31. 15. Gümüs H, Bükte Y, Özdemir E, et al. Variations of the celiac trunk and hepatic arteries: a study with 64-detector computed tomographic angiography. Eur Rev Med Pharmacol Sci. 2013;17:1636–41. 16. Iezzi R, Cotroneo AR, Giancristofaro D, et al. Multidetector-row CT angiographic imaging of the celiac trunk: anatomy and normal variants. Surg Radiol Anat. 2008;30:303–10. 17. Saylisoy S, Atasoy Ç, Ersöz S, et al. Multislice CT angiography in the evaluation of hepatic vascular anatomy in potential right lobe donors. Diagn Interv Radiol. 2005;11:51–9. 18. Song SY, Chung JW, Yin YH, et al. Celiac axis and common hepatic artery variations in 5002 patients: systematic analysis with spiral CT and DSA. Radiology. 2010;255:278–88. 19. Reis FRS, Cardia PP, D’Ippolito G. Computed tomography angiography in patients with active gastrointestinal bleeding. Radiol Bras. 2015;48:381–90. 20. Erbay N, Raptopoulos V, Pomfret EA, et al. Living donor liver transplantation in adults: vascular variants important in surgical planning for donors and recipients. ARJ Am J Roentgenol. 2003;181:109–14. 21. Schmidt S, Demartines N, Soler L, et al. Portal vein normal anatomy and variants: implication for liver surgery and portal vein embolization. Semin Intervent Radiol. 2008;25:86–91. 22. Soares RV, Coelho JCU, Matias JEF, et al. Anatomia da artéria hepática em doadores e receptores de transplante hepático intervivos. Rev Col Bras Cir. 2006;33:63–7. 23. Araujo-Neto SA, Mello-Júnior CF, Franca HA, et al. Multidetector computed tomography angiography of the celiac trunk and hepatic arterial system: normal anatomy and main variants. Radiol Bras. 2016;49:49–52. 24. Giardino A, Miller FH, Kalb B, et al. Hepatic epithelioid hemangioendothelioma: a report from three university centers. Radiol Bras. 2016;49:288–94. 25. Cruz JF, Cruz MAF, Machado Neto J, et al. Prevalence and sonographic changes compatible with fatty liver disease in patients referred for abdominal ultrasound examination in Aracaju, SE. Radiol Bras. 2016;49:1–5. 26. Siqueira GRS, Guimarães MD, Franco LFS, et al. Exophytic hepatocellular carcinoma, simulating a mesenchymal tumor, in a noncirrhotic liver. Radiol Bras. 2017;50:62–3. 27. Staziaki PV, Teixeira BC, Pedrazzani BM, et al. Hepatoblastoma with solid and multicystic aspect mimicking a mesenchymal hamartoma: imaging and anatomopathologic findings. Radiol Bras. 2017;50:68. 28. Ramalho M, Matos AP, AlObaidy M, et al. Magnetic resonance imaging of the cirrhotic liver: diagnosis of hepatocellular carcinoma and evaluation of response to treatment – Part 1. Radiol Bras. 2017; 50:38–47. 29. Ramalho M, Matos AP, AlObaidy M, et al. Magnetic resonance imaging of the cirrhotic liver: diagnosis of hepatocellular carcinoma and evaluation of response to treatment – Part 2. Radiol Bras. 2017; 50:115–25. 30. Freitas ACT, Coelho JCU, Matias JEF, et al. Anatomia arterial hepática: estudo em 150 transplantes hepáticos. Rev Col Bras Cir. 2000;28:13–6. 31. Panagouli E, Venieratos D, Lolis E, et al. Variations in the anatomy of the celiac trunk: a systematic review and clinical implications. Ann Anat. 2013;195:501–11. 32. Chen H, Yano R, Emura S, et al. Anatomic variation of the celiac trunk with special reference to hepatic artery patterns. Ann Anat. 2009;191:399–407. 33. Araujo-Neto SA, Franca HA, Mello-Júnior CF, et al. Anatomical variations of the celiac trunk and hepatic arterial system: an analysis using multidetector computed tomography angiography. Radiol Bras. 2015;48:358–62. 34. Özbülbül NI. CT angiography of the celiac trunk: anatomy, variants and pathologic findings. Diagn Interv Radiol. 2011;17:150–7 1. PhD, Adjunct Professor of Clinical Surgery, School of Medicine, Universidade Estadual do Ceará (UECE), Head of the Liver Transplant Program at the Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil 2. Medical Student at the Universidade Estadual do Ceará (UECE), Fortaleza, CE, Brazil 3. PhD, Substitute Professor of Anatomy, School of Medicine, Universidade Estadual do Ceará (UECE), Fortaleza, CE, Brazil 4. PhD, Adjunct Professor of Diagnostic Imaging, School of Medicine, Universidade Estadual do Ceará (UECE), Fortaleza, CE, Brazil 5. MD, General Surgeon, Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil Mailing address: Igor Farias Araujo Rua Joaquim Lima, 1315, ap. 701, Papicu Fortaleza, CE, Brazil, 60175-005 E-mail: igor_farias98@hotmail.com Study conducted in the Department of Anatomy and Radiology, School of Medicine, Universidade Estadual do Ceará (UECE), and at the Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil. Received October 3, 2016 Accepted after revision January 2, 2017. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554