Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 51 nº 2 - Mar. / Apr. of 2018
Vol. 51 nº 2 - Mar. / Apr. of 2018
|
ICONOGRAPHIC ESSAY
|
|
Computed tomography and magnetic resonance imaging findings in infants with microcephaly potentially related to congenital Zika virus infection |
|
|
Autho(rs): Aníbal Araujo Alves Peixoto Filho1; Simone Baltar de Freitas1; Márcio Morikoshi Ciosaki1; Lourenço Nogueira e Oliveira1; Onildo Tavares dos Santos Júnior1 |
|
|
Keywords: Microcephaly; Zika virus infection; Tomography, X-ray computed; Magnetic resonance imaging. |
|
|
Abstract: INTRODUCTION
States in several parts of the northeastern region of Brazil have recorded an unusual increase in the number of infants born with microcephaly, an urgent public health problem that affects the quality of life of children and their families. The situation has recently been declared a public health emergency of international concern(1). Zika virus infection in humans was first identified in Uganda and Tanzania in 1952, subsequent outbreaks being reported in other parts of Africa, as well as in the Americas, Asia, and the Pacific(2). However, only recently, in large outbreaks in French Polynesia in 2013 and in Brazil in 2015, neurological and autoimmune complications have been reported, as has the current association with microcephaly(3,4). The elucidation of the etiological factor responsible for this most recent outbreak involves, among other factors, the recognition of the relationship between the presence of the virus and the occurrence of microcephaly; verification of the virus crossing the placental barrier; and identification of the Zika virus in stillborn and newborn infants with microcephaly or other malformations of the central nervous system(3). The virus has been identified in the amniotic fluid of pregnant women following the ultrasound diagnosis of microcephaly(5), in the brain tissue of a fetus aborted at 32 weeks of gestation in Slovenia(4), and in a neonate that evolved to death in the northeastern Brazilian state Ceará(3). According to the World Health Organization(6), imaging examinations are necessary for the detection of structural abnormalities in the brains of children born with microcephaly. EMBRYOLOGY In brief, the complex embryological process of brain development involves neurulation, followed by neuronal proliferation, neuronal migration, organization (formation of the opercula, sulci, and gyri), and, finally, myelination. That process begins in the third week of gestation and continues until after birth. The process can be impeded by events of different natures, which, depending on the severity of the insult, can cause microcephaly. Microcephaly can be primary (genetic) or secondary, the most common causes of secondary microcephaly being vascular disorders, maternal diabetes, trauma, and infections(7). CLINICAL ASPECTS The images presented in this study were obtained from the examinations of nine infants admitted to a rehabilitation hospital with microcephaly apparently related to congenital Zika virus infection, according to the criteria established by local authorities(3). The infants studied were between 1 and 7 months of age at the time of the examination. All of their mothers had reported having had a cutaneous rash between the second and fourth months of gestation. The serology performed during pregnancy did not identify another infectious factor that could be the cause of the microcephaly. The infants underwent computed tomography (CT) and magnetic resonance imaging (MRI) without sedation, with guidelines related to sleep deprivation. IMAGING FINDINGS Various congenital infections, although not pathognomonic, share some imaging characteristics, chief among which are calcifications. Other findings, such as ventriculomegaly, posterior fossa alterations, and malformations of cortical development, have been reported(3). Below, we describe the main imaging findings among our patients with microcephaly. Parenchymal calcifications In all of the patients included, we observed parenchymal calcifications, varying in number and location, that were characterized by hyperattenuating foci on CT scans (Figure 1) and by areas of low signal intensity in gradient-echo MRI sequences (Figure 2). Some of the calcifications also showed high signal intensity in fast spin-echo and fast spoiled gradient echo T1-weighted sequences. 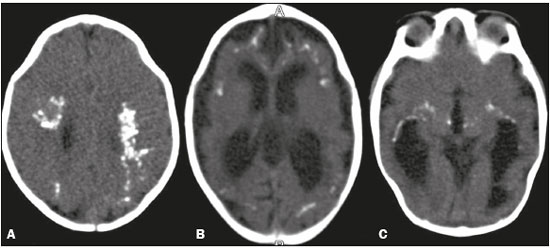 Figure 1. CT scan showing parenchymal calcifications in several locations in different patients. A: In the deep white matter and in cortical-subcortical regions, at the level of the corona radiata, assuming a confluent aspect. B: In cortical-subcortical regions, at the level of the lateral ventricles. C: Calcifications in the thalamus and in the capsulonuclear regions. Note the narrowing of the frontal bones, in A, and the small left frontal subcortical cyst, in B. 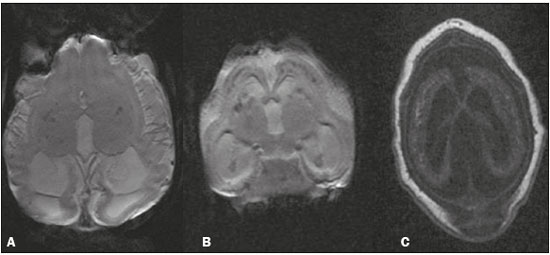 Figure 2. MRI. A,B: Volumetric gradient-echo sequences showing foci of signal hypointensity in the cortical-subcortical regions, thalamic, and capsulonuclear regions. C: Volumetric fast spoiled gradient-echo T1-weighted sequence, of the same patient depicted in B, showing foci of signal hyperintensity, confluent in the cortical-subcortical regions, corresponding to the foci of signal hypointensity seen in the gradient-recalled echo sequence. Calcifications were often seen in cortical-subcortical regions, either in a linear arrangement or confluent (Figure 1A). Several calcifications were also identified in the deep white matter, periventricular white matter, and deep gray matter (Figure 1C). Alterations in the morphology of the parenchyma and gyri We identified alterations in the gyral pattern, a simplified pattern, characterized by few gyri and shallow sulci, predominating throughout the parenchyma (Figure 3). We also identified alterations on the lissencephaly spectrum (Figure 4), with cortical thickening, greater scarcity (or even the absence) of gyri, and a nearly smooth parenchymal surface, seen in a more diffuse or localized form. In other infants, we observed areas of polymicrogyria accompanied by gyral simplification (Figure 3B). Several patients presented a marked reduction in parenchymal volume, ventriculomegaly being quite common and, in some cases, accompanied by enlargement of the subarachnoid spaces. 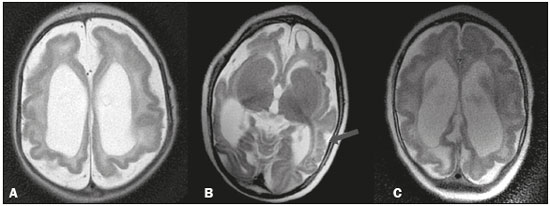 Figure 3. MRI, T2-weighted sequences in different patients, showing a pattern of gyral simplification, accompanied by ventriculomegaly and enlargement of the subarachnoid spaces. In B, a subcortical cyst can be seen in the left frontal region, as can polymicrogyria, which is best visualized in the left temporoparietal region (arrow). 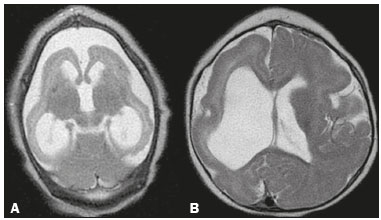 Figure 4. MRI scan showing patterns of altered gyral morphology on the lissencephaly spectrum, characterized by smoother contours of the cortical surface and a certain thickening, with a more generalized presentation in A and an asymmetric presentation in B, with more pronounced pachygyria in the right frontal region. Alterations in the corpus callosum In all of the examinations included in this study, we observed changes in the corpus callosum, characterized by hypogenesis (Figure 5) or agenesis (Figure 6), with or without significant hypoplasia. Consequently, in some cases—those in which the agenesis or hypogenesis was more pronounced—there was a predominance of colpocephaly of the lateral ventricles (Figure 5A).  Figure 5. MRI: axial T2-weighted sequence (A) showing hypogenesis of the corpus callosum; and sagittal three-dimensional fast imaging employing steady-state acquisition sequence (B), showing more clearly the genu and body of the corpus callosum, both of which are hypoplastic. 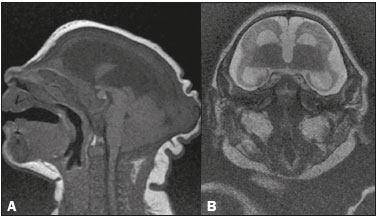 Figure 6. MRI: sagittal T1-weighted sequence (A) and coronal T2-weighted sequence (B), both showing agenesis of the corpus callosum. In A, note the craniofacial disproportion, occipital bone protuberance ("saddling"), skin folds, and caudal projection of the cerebellar tonsils. In B, note the high positioning of the third ventricle and the absence of the corpus callosum, as well as enlargement of the subarachnoid space, ventriculomegaly, and considerable reduction in the size of the telencephalon. Other alterations We identified changes in the posterior fossa (Figure 7), including hypoplasia of the right cerebellar hemisphere and some changes on the Dandy-Walker continuum. In one of the infants, we observed a subcortical cyst (Figure 3B). In the cranial vault, we identified occipital protuberance (Figures 5B and 6A) and narrowing of the frontal bones (Figure 1A). 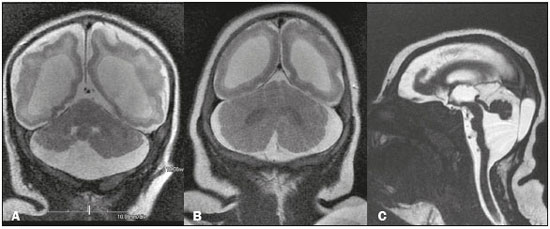 Figure 7. MRI. A,B: Coronal T2-weighted sequence showing discrete hypoplasia of the right cerebellar hemisphere (in A) and relative prominence of the cerebellum in relation to the telencephalon (in B), as well as (in both) ventriculomegaly and a significant reduction in the volume of the white matter. C: Hypoplasia and rotation of the cerebellar vermis, accompanied by a prominent cerebrospinal fluid collection in the posterior fossa, as well as changes on the Dandy-Walker continuum. Note that there is also hypoplasia of the brainstem, notably of the pons. CONCLUSION Due to the significant increase in the number of infants born with microcephaly, neuroimaging examinations have become an indispensable tool for investigating the morphology of the brain parenchyma of such infants. In this essay, we have illustrated the main imaging findings, in the initial examinations carried out at our institution, in infants with microcephaly that was apparently related to congenital infection with the Zika virus. REFERENCES 1. Heymann DL, Hodgson A, Sall AA, et al. Zika virus and microcephaly: why is this situation a PHEIC? Lancet. 2016;387:719–21. 2. World Health Organization. Media centre. Zika virus. [Internet]. 2016. [updated 2016 June 2; cited 2016 Jul 15]. Available from: http://www.who.int/mediacentre/factsheets/zika/en/. 3. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Protocolo de vigilância e resposta à ocorrência de microcefalia e/ou alterações do sistema nervoso central (SNC). Emergência de saúde pública de importância internacional – ESPII. [Internet]. Brasília: Ministério da Saúde, 2016. [updated 2016 Mar 10; cited 2016 Jul 15]. Available from: http://combateaedes.saude.gov.br/images/sala-de-situacao/Microcefalia-Protocolo-de-vigilancia-e-resposta-10mar2016-18h.pdf. 4. Mlakar J, Korva M, Tul N, et al. Zika virus associated with microcephaly. N Engl J Med. 2016;374:951–8. 5. Oliveira Melo AS, Malinger G, Ximenes R, et al. Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the iceberg? Ultrasound Obstet Gynecol. 2016;47:6–7. 6. Organização Mundial da Saúde. Avaliação de bebés com microcefalia no contexto do vírus Zika: orientações provisórias. [Internet]. [updated 2016 Mar 4; cited 2018 Feb 15]. Available from: http://apps.who.int/iris/bitstream/10665/204475/8/WHO_ZIKV_MOC_16.3_por.pdf?ua=1). 7. Osborn AG. Encéfalo de Osborn: imagem, patologia e anatomia. Porto Alegre, RS: Artmed; 2014. MD, Specialist in Radiology and Diagnostic Imaging for the Rede Sarah de Hospitais de Reabilitação, Salvador, BA, Brazil Study conducted in the Rede Sarah de Hospitais de Reabilitação, Salvador, BA, Brazil. Mailing address: Dr. Aníbal Araujo Alves Peixoto Filho Associação das Pioneiras Sociais – Setor de Radiologia Avenida Tancredo Neves, 2782, Caminho das Árvores Salvador, BA, Brazil, 41820-900 E-mail: anibalpeixotof@gmail.com Received July 29, 2016. Accepted after revision August 21, 2016. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554