Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 52 nº 1 - Jan. /Feb. of 2019
Vol. 52 nº 1 - Jan. /Feb. of 2019
|
LETTERS TO THE EDITOR
|
|
Congenital lobar emphysema |
|
|
Autho(rs): Tiago Kojun Tibana1; Denise Maria Rissato Camilo2; Thiago Franchi Nunes3; Edson Marchiori4 |
|
|
Dear Editor,
A 41-day-old male infant was born by cesarean section, without complications, at 38 weeks of gestation. The results of the prenatal examinations had been normal, and postnatal nutrition was exclusively from breastfeeding. He was referred to our facility with a history of progressive respiratory distress, which had started on postnatal day 7 and had worsened three days prior to the consultation. He was afebrile. The parents reported having previously sought treatment more than once and having received a prescription for nebulization, which resulted in partial improvement of the condition. The initial physical examination revealed subcostal retraction, diminished breath sounds on the right side and diffuse wheezing on the left. The respiratory rate was 72 breaths/min, and the oxygen saturation on room air was 96%. A chest X-ray (Figure 1A) showed right-sided hyperlucency, with a mediastinal shift to the left. Computed tomography (CT) revealed hyperinflation of the middle lobe parenchyma, the expansion of which was displacing the mediastinum to the left (Figures 1B, 1C, and 1D). The patient was treated with a nebulized bronchodilator and oxygen therapy, which resulted in clinical improvement and stabilization of the condition. At five days after admission, he was asymptomatic and was discharged to outpatient follow-up. 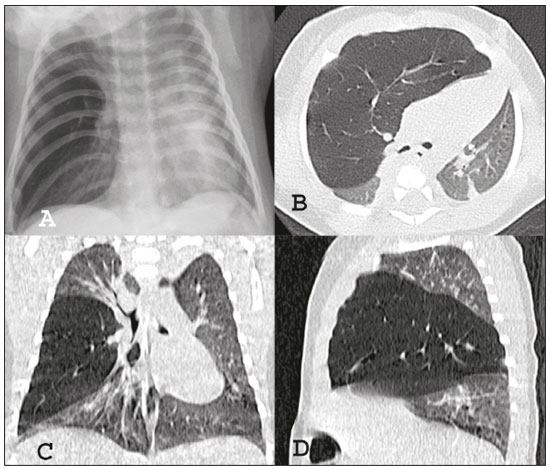 Figure 1. Chest X-ray in anteroposterior view (A) showing hyperlucency of the right hemithorax with a mediastinal shift to the left. Noncontrast chest CT, in axial, coronal, and sagittal slices (B, C, and D, respectively), showing hyperinflation of the middle lobe and expansion of the mediastinal structures. Congenital diseases have been the subject of recent publications in the area of radiology(1-4). Congenital lobar emphysema (CLE) is a rare pulmonary malformation whose main cause is probably developmental anomalies of the bronchial cartilage. Less common causes include extrinsic airway compression, usually caused by idiopathic bronchial stenosis, mucus plugging, or vascular malformations. However, in approximately half of all cases, the cause goes undetermined(5-10). CLE is characterized by progressive lobar hyperinflation, caused by air trapping in a collapsed airway, resulting in distension of the lobe and a mass effect that compresses the other lobes and shifts the mediastinum(6,7). There is no alveolar destruction(11). CLE involves the left upper lobe in 42.2% of cases, the right middle lobe in 35.3%, the right upper lobe in 20.7%, and the lower lobes in less than 1.0%(11,12). Its clinical presentation ranges from mild respiratory dysfunction to acute respiratory failure. Most patients are diagnosed within the first month of life, showing a moderate degree of respiratory dysfunction in the immediate postnatal period, and present symptoms before reaching six months of age, with progressive worsening due to increased pulmonary hyperinflation. Some patients remain asymptomatic for years(5,10,11). A diagnosis of CLE is generally suspected in a child with respiratory failure in whom a chest X-ray reveals hyperinflation of a lung lobe, with or without contralateral pulmonary herniation, and a contralateral mediastinal shift(7,10). CT is an excellent imaging modality for excluding diagnoses of a subjacent hilar mass and alterations in the bronchial lumen. In addition, it can accurately delineate and localize the lesion, which is particularly useful for preoperative evaluation. CT usually shows hyperinflation of a lung lobe and attenuation of the bronchovascular bundle, which runs along the periphery of the expanded alveoli(10,11). The differential diagnosis includes pneumatocele, pneumothorax, pulmonary atelectasis, and pulmonary hypoplasia. CLE is generally considered an indication for surgery, lobectomy being the procedure of choice in symptomatic patients(5,10). For patients who exhibit mild respiratory distress, conservative treatment is an option(3). REFERENCES 1. Werner H, Daltro P, Fazecas T, et al. Prenatal diagnosis of sirenomelia in the second trimester of pregnancy using two-dimensional ultrasound, three-dimensional ultrasound and magnetic resonance imaging. Radiol Bras. 2017;50:201-2. 2. Duarte ML, Silva AQP, Alvarenga SB, et al. Giant cyamella: a rare sesamoid bone. Radiol Bras. 2017;50:270-1. 3. Duarte ML, Duarte ER, Solorzano DB, et al. Spondylometaphyseal dysplasia: an uncommon disease. Radiol Bras. 2017;50:63-4. 4. Niemeyer B, Muniz BC, Gasparetto EL, et al. Congenital Zika syndrome and neuroimaging findings: what do we know so far? Radiol Bras. 2017;50:314-22. 5. Hochhegger B, Irion KL, Andrade CF, et al. Congenital lobar emphysema: the role of multislice computed tomography with virtual bronchoscopy in the differential diagnosis with bronchial foreign bodies. Eur Arch Otorhinolaryngol. 2012;269:2015-6. 6. Nayar PM, Thakral CL, Sajwani MJ. Congenital lobar emphysema and sequestration-treatment by embolization. Pediatr Surg Int. 2005;21: 727-9. 7. Biyyam DR, Chapman T, Ferguson MR, et al. Congenital lung abnormalities: embryologic features, prenatal diagnosis, and postnatal radiologic-pathologic correlation. Radiographics. 2010;30:1721-38. 8. Wright C. Congenital malformations of the lung. Current Diagnostic Pathology. 2006;12:191-201. 9. Maiya S, Clarke JR, More B, et al. Bilateral congenital lobar emphysema: how should we proceed? Pediatr Surg Int. 2005;21:659-61. 10. Reiss I, van de Ven CP, Tibboel D. Congenital lung malformations. Diagnostic and therapeutic approaches. Intensivmed. 2008;45:12-8. 11. Wasilewska E, Lee EY, Eisenberg RL. Unilateral hyperlucent lung in children. AJR Am J Roentgenol. 2012;198:W400-14. 12. Stigers KB, Woodring JH, Kanga JF. The clinical and imaging spectrum of findings in patients with congenital lobar emphysema. Pediatr Pulmonol. 1992;14:160-70. 1. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; a. https://orcid.org/0000-0001-5930-1383 2. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; b. https://orcid.org/0000-0002-9016-8610 3. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; c. https://orcid.org/0000-0003-0006-3725 4. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil; d. https://orcid.org/0000-0001-8797-7380 Correspondence: Dr. Edson Marchiori Rua Thomaz Cameron, 438, Valparaíso Petrópolis, RJ, Brazil, 25685-120 Email: edmarchiori@gmail.com Received August 14, 2017 Accepted after revision September 14, 2017 |
|
GN1© Copyright 2024 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554