Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 52 nº 3 - May / June of 2019
Vol. 52 nº 3 - May / June of 2019
|
LETTERS TO THE EDITOR
|
|
Pleuropulmonary blastoma manifesting as spontaneous pneumothorax: an unusual presentation |
|
|
Autho(rs): Isa Félix Adôrno1; Rômulo Florêncio Tristão Santos1; Bernardo Bacelar de Faria2; Edson Marchiori3; Thiago Franchi Nunes1 |
|
|
Dear Editor,
A previously healthy two-year-old female patient presented to the emergency department with sudden-onset dyspnea and right-sided chest pain. Physical examination revealed tachypnea, absence of breath sounds on the right and distention of the ipsilateral jugular vein. Routine laboratory tests showed no abnormalities. A chest X-ray showed hypertensive pneumothorax on the right. A computed tomography (CT) scan of the chest revealed, in addition to the voluminous pneumothorax, extensive cavitation and atelectasis in the right lung (Figures 1A, 1B, and 1C). We opted for thoracic surgery involving immediate drainage of the pneumothorax and, during the same hospitalization, resection of the pulmonary lesion. The macroscopic pathological examination revealed a circumscribed, subpleural, nodular lesion that was solid-cystic and friable, measuring 1.4 cm in diameter, together with pleural rupture. Histologically, we also observed a neoplasm with foliaceous and solid patterns, together with cystic areas, lined with normal respiratory epithelium (Figure 1D). The neoplastic cells presented two predominant patterns: an undifferentiated immature (blastomatous) component, mainly in the subepithelial region; and a spindle cell component with rhabdomyoblastic differentiation, comprising a few anaplastic cells and numerous atypical mitoses. We observed no chondral differentiation or necrosis. The final diagnosis was type II pleuropulmonary blastoma (PPB). The subsequent staging did not reveal any metastatic dissemination of the disease. After surgery, the patient recovered quickly, with no respiratory symptoms. A follow-up chest X-ray showed full expansion of the affected lung. There was no need for postoperative radiotherapy. 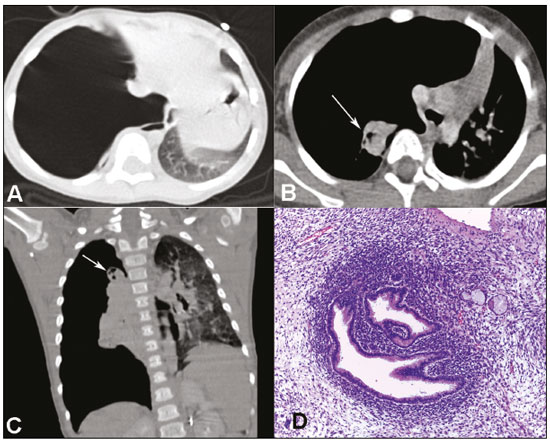 Figure 1. CT scan of the chest showing a voluminous pneumothorax on the right (A), extensive cavitation (arrows), and atelectasis of the right lung (B,C). D: Histological section showing the biphasic component of the neoplasm: the solid area with a dense immature component around the normal pulmonary epithelium (cambium layer); and the adjacent spindle-cell component in which there were typical cytoplasmic striations (not shown). Hematoxylin-eosin staining (magnification, ×200). PPB is an aggressive intrathoracic malignant neoplasm that mainly affects children under five years of age and, although rare, is the most common primary malignant neoplasm of the lung in childhood(1). It derives from primitive embryonic cells that arise during the development of the lung, similar to what is observed in other childhood neoplasms. These primitive cells are associated with other congenital pulmonary cystic malformations, some of which evolve to an aggressive neoplasm, with possible sarcomatous transformation, demonstrating the potential of multidirectional differentiation of stem cells(2). In general, PPB manifests as an intrapulmonary subpleural mass and is characterized histologically by primitive blastomatous and sarcomatous differentiation containing non-neoplastic pulmonary epithelial elements. With the development of new technologies, imaging studies are becoming increasingly more important in pediatrics(3-7). However, there have been few articles describing the imaging findings of PPB(8). Pneumothorax is a common presentation in type I (purely cystic) PPB and type II (mixed) PPB(9,10). PPB is highly aggressive in its type III (solid) form, with recurrence and metastases. The most common metastases are those to the lung/pleura, central nervous system, and musculoskeletal system. Although CT of the chest is the most widely used technique for investigating a pulmonary mass, magnetic resonance imaging is useful because it can better demonstrate the origin of the mass, its anatomical relationships, and the involvement of adjacent structures. Radiographic findings, in general, are not sufficient for a definitive diagnosis, lung biopsy being essential for the final diagnosis. REFERENCES 1. Orazi C, Inserra A, Schingo PM, et al. Pleuropulmonary blastoma, a distinctive neoplasm of childhood: report of three cases. Pediatr Radiol. 2007;37:337-44. 2. Messinger YH, Stewart DR, Priest JR, et al. Pleuropulmonary blastoma: a report on 350 central pathology-confirmed pleuropulmonary blastoma cases by the International Pleuropulmonary Blastoma Registry. Cancer. 2015;121:276-85. 3. Vilela VM, Ribeiro VM, Paiva JC, et al. Clinical and radiological characterization of fibrous hamartoma of infancy. Radiol Bras. 2017;50:204-5. 4. Moreira FP, Aihara AY, Lederman HM, et al. Cognitive map to support the diagnosis of solitary bone tumors in pediatric patients. Radiol Bras. 2018;51:297-302. 5. Peçanha AS, Monteiro AM, Gazolla FM, et al. Ultrasound as a method to evaluate the distribution of abdominal fat in obese prepubertal children and the relationship between abdominal fat and metabolic alterations. Radiol Bras. 2018;51:293-6. 6. Figueiras FN, Duarte ML, Duarte ER, et al. Giant ovarian teratoma: an important differential diagnosis of pelvic masses in children. Radiol Bras. 2017;50:342-3. 7. Togni Filho PH, Casagrande JLM, Lederman HM. Utility of the inspiratory phase in high-resolution computed tomography evaluations of pediatric patients with bronchiolitis obliterans after allogeneic bone marrow transplant: reducing patient radiation exposure. Radiol Bras. 2017;50:90-6. 8. Naffaa LN, Donnelly LF. Imaging findings in pleuropulmonary blastoma. Pediatr Radiol. 2005;35:387-91. 9. Kuzucu A, Soysal O, Yakinci C, et al. Pleuropulmonary blastoma: report of a case presenting with spontaneous pneumothorax. Eur J Cardiothorac Surg. 2001;19:229-30. 10. Piastra M, Ruggiero A, Caresta E, et al. Critical presentation of pleuropulmonary blastoma. Pediatr Surg Int. 2005;21:223-6. 1. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0002-2106-1211 2. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0002-8679 3. Screenlab, Campo Grande, MS, Brazil; https://orcid.org/0000-0002-4258-2198 4. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil; https://orcid.org/0000-0001-8797-7380 5. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0003-0006-3725 Correspondence: Dr. Edson Marchiori Rua Thomaz Cameron, 438, Valparaiso Petrópolis, RJ, Brazil, 25685-120 Email: edmarchiori@gmail.com Received October 17, 2017 Accepted after revision November 08, 2017 |
|
GN1© Copyright 2024 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554