Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 3 - May / June of 2010
Vol. 43 nº 3 - May / June of 2010
|
ORIGINAL ARTICLE
|
|
Fetal and placental Doppler velocimetry in hypertensive pregnant women and perinatal outcomes according to gestational age |
|
|
Autho(rs): Pedro Pires, Aníbal Eusébio Faúndes Latham, Suellene Keylla de Magalhães Mabessone, Ana de Fátima de Azevedo Ferreira, Fabiana Gomes de Souza Rodrigues, Janaina Souza Leon, Juliana Limeira de Moura Ramos |
|
|
Keywords: Doppler velocimetry, Hypertension, Perinatal outcome |
|
|
Abstract:
IPhD, Coordinator for Unit of Fetal Medicine, Maternal-Neonatal Department - Faculdade de Ciências Médicas da Universidade de Pernambuco (UPE), Recife, PE, Brazil
INTRODUCTION Currently, one of the main preoccupations in obstetrics is to assure good vitality conditions for the fetus at risk. Such preoccupation is even greater in the presence of maternal diseases that are known to cause placental insufficiency and intrauterine growth restriction (IUGR) as is the case, mainly, of arterial hypertension(1). This is the clinical entity that is mostly associated with IUGR and placental insufficiency(2-7). The Doppler technique allows the noninvasive study of the uterine and fetoplacental circulation, allowing the early diagnosis of hypoxia states and the prediction of adverse perinatal outcomes(6,8-10). The Doppler scan allows the analysis of the main vessels resistance index, with the most utilized ones being the umbilical artery and the middle cerebral artery(11-14). In the compensation phase of hypoxia, the placental resistance increases and the umbilical arteries resistance indices rise. Subsequently, a progressive reduction of the cerebral vascular resistance is observed, progressing to "centralization". Such phenomenon precedes severe fetal involvement by 10 to 12 days, with fetal acidosis and higher perinatal morbimortality(6). Alterations in the Doppler pattern of the umbilical artery, particularly absent or reversed diastolic flow, are indicative of placental dysfunction(15), with high risk of fetal distress and, particularly, vulnerability to prematurity complications(16), which determines a balance between fetal risk versus neonatal risk in the identification of the appropriate moment for intervention(17-19). For some authors, obstetric management is still predominantly based on the umbilical artery Doppler analysis(4,18,20-22), although some studies point towards the inclusion of more than one vessel in the assessment of vitality of fetuses at risk(7,23). It is important to highlight that severe dopplervelocimetric alterations indicative of intensive fetal monitoring or interruption occur in premature fetuses, particularly in cases of extreme prematurity(24). With the purpose of clarifying the capability of different Doppler indicators to predict the risk of perinatal complications, the authors have simultaneously evaluated the risk of bad perinatal outcomes in the presence of dopplervelocimetric changes in the umbilical artery, middle cerebral artery and in the umbilical-cerebral indices. At the same time, the authors have evaluated the occurrence of substantial changes in results after control according to gestational age at birth.
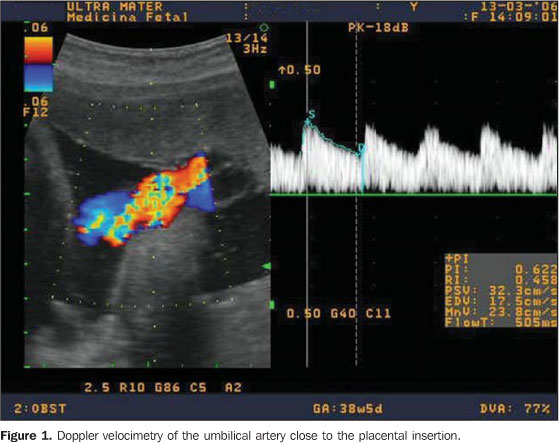
MATERIALS AND METHODS The initial series comprised 497 hypertensive pregnant women in the period from January 2002 to August 2006. For the studies of the fetoplacental circulation, a Shimadzu ultrasonography unit model SDU-2200 (Shimadzu; Kyoto, Japan) with a Doppler device with color blood flow mapping and a 3.5 MHz convex transducer, was utilized. The window filter was set between 50 and 100 Hz. With the patient lying in semi-Fowler position and in the absence of body motion and fetal breathing movements, utilizing real-time images, the blood flow color mapping was initiated, thus obtaining the color mapping of the vessels to be studied, which were evaluated by means of the Doppler device, with adjustments of the sample volume for each vessel, in the absence of fetal movements. The Doppler scan of the umbilical artery was performed in open loop, close to the placental insertion and insonation angle always below 60°. The spectral analysis was considered appropriate in cases where at least three similar velocity waves were observed in the same spectrum (Figure 1). The analysis was considered as abnormal in cases where the diastole was absent or reversed in the umbilical artery, or the pulsatility index was above the 95th percentile(25).
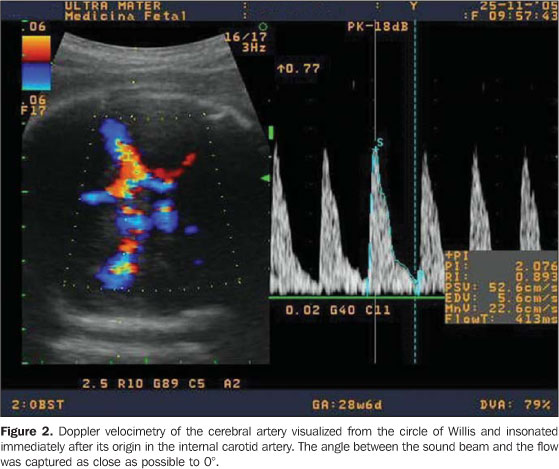
The middle cerebral artery was visualized from the circle of Willis and was insonated immediately after its origin in the internal carotid artery. The angle between the sound beam and the flow was captured the closest possible to 0°, with the pulsatility index being measured (Figure 2). A middle cerebral artery pulsatility index (MCAPI) < 5th percentile and umbilical artery/cerebral artery (UAPI/MCAPI) ratio > 95th percentile for the gestational age were considered as abnormal(25).
Exclusion criteria were the following: cases with intervals between the last dopplervelocimetric study and the labor > 7 days, absence of data on perinatal outcomes at birth, presence of congenital defects or fetal or neonatal chromosomal abnormalities, maternal disease leading to congenital infection, and gestational age at birth < 24 weeks. With these criteria, 208 patients were excluded, so the final sample included the remaining 289 pregnant women. The software EPI-Info, version 1.0 was utilized for data organization. The cases were divided into three gestational age groups (< 33 weeks, 33 to 36 weeks and > 37 weeks) and classified according to the presence or absence of each adverse perinatal outcome as follows: Apgar score at the 5th minute < 7; newborn small for gestational age (SGA); occurrence of neonatal hypoxic-ischemic syndrome (HIS); occurrence of respiratory distress syndrome (RDS) and perinatal death. A prospective analysis of risk of bad perinatal outcomes calculated by the relative estimated risk (odds ratio) of the studied outcomes was performed, in accordance with results of Doppler velocimetry performed up to seven days before the labor. Later, the same calculation was carried out, this time adjusted according to gestational age. The present study was developed in compliance with Resolution 196/1996 of Conselho Nacional de Saúde (Brazilian Council of Health), and the recommendations of the Helsinki Declaration VI for research with humans, and was duly submitted and approved by the Committee for Ethics in Research of Centro Integrado de Saúde Amaury de Medeiros of Universidade de Pernambuco.
RESULTS Sample characteristics The patients' ages ranged from 14 to 43 years (mean age, 26 years); with respect to parity, 57.1% of the women were primigravidas. Nearly two thirds of cases corresponded to preeclampsia. Vaginal deliveries comprised only 25.6% of the cases. The last Doppler scan was performed up to one day before delivery in 51.2% of the cases (Table 1).
In almost two thirds of the cases the newborns were preterm, and among them 27.7% had less than 33 weeks of gestational age at birth. The newborns weight ranged from 550 g to 4,580 g. In 21.5%, the Apgar scores were < 7 at the 5th minute, and 31.5% of the cases were SGA. Almost 20% of the neonates presented HIS and 16%, RDS. Fetal death occurred in 2%, and neonatal death in 6.5% of cases (Table 2).
Association between the dopplervelocimetric results and perinatal outcomes No association was observed between UAPI, MCAPI and of the UAPI/MCAPI ratio and Apgar score < 7 at the 5th minute before the adjustment for gestational age. After the adjustment, the risk of Apgar < 7 at the 5th minute was more than two times and almost twice higher in fetuses in whom the UAPI and MCAPI, respectively, were altered. However, only the association with UAPI alteration reached statistical significance (Table 3).
The authors observed that alterations in UAPI, MCAPI and UAPI/MCAPI ratio increased from five to seven times the risk of the occurrence of SGA newborns in the analysis without adjustment and around three times in the adjusted analysis according to gestational age (Table 4). The increase in risk was statistically significant for all studied dopplervelocimetric parameters.
Alterations in UAPI, MCAPI and in the UAPI/MCAPI ratio increased two to five times the risk of HIS before adjustment, and between one and one half and more than three and a half times after the adjustment according to gestational age. The increase in the adjusted risk was significant only for UAPI and the UAPI/MCAPI ratio (Table 5).
The observed increase in the risk of RDS in cases with altered UAPI, MCAPI and UAPI/MCAPI ratio was between two and six times in the analysis without adjustment. However, after adjustment by gestational age, no increase was observed in the risk of this neonatal complication in the cases with these alterations at Doppler (Table 6).
In spite of the fact that the gross risk of perinatal mortality having been between three to ten times greater in cases with alterations in UAPI, MCAPI and UAPI/MCAPI ratio in the analysis adjusted according to gestational age, only the altered UAPI presented a statistically significant risk almost three times higher for perinatal death (Table 7).
Table 8 shows the summarized results for a better visualization and comparison of the different indicators of Doppler alterations. It can be observed that the UAPI is the best indicator o risk of bad perinatal outcomes, particularly when the risk evaluation is adjusted by gestational age of the neonate.
DISCUSSION The results of the present study suggest that the evaluation of blood flow in the umbilical artery was the best indicator of risk of adverse perinatal outcome, as compared with the evaluation of the middle cerebral artery and with the IAPI/MCAPI ratio. Before the adjustment for gestational age, the three indicators seem to have a similar capability of predicting adverse perinatal outcomes. It is important to note that the increase in risk was always greater when one considers the Doppler results for the umbilical artery compared with the ones for the middle cerebral artery. It should be highlighted that the difference between these two indicators is more noticeable when one observes the risks of adverse perinatal outcomes after adjustment for gestational age. Various authors have not considered the factor of gestational age in their studies(7,9,11,13,18,26). In the present study, alterations in UAPI allowed the prediction of a higher risk (about three times higher) in four out of five indicators of the adverse perinatal outcomes studied. For RDS, the risk was 50% higher, but it was not statistically significant. In contrast, MCAPI alterations allowed the prediction of a higher risk only for SGA, and alterations in the UAPI/MCAPI ratio allowed predictions only for SGA and HIS. For some authors, the study of more than one vessel contributes to improve the diagnosis of the fetal situation, evaluating the Doppler velocimetry capability to predict perinatal outcomes, including only fetuses with confirmed IURG diagnosis(3,6,7,12,27,28). In the present study, hypertensive pregnant women were included, as it may lead to placental insufficiency potentially presenting a risk of fetal damage, without being necessarily present. Another important information is related to the evaluation of perinatal outcomes in cases with zero diastole or reversed flow, which are severe alterations in the dopplervelocimetric pattern(9,10,13,26). The present study considered not only absent or reversed diastole as altered results of the umbilical artery, but also cases in which the pulsatility indices were above the 95th percentile. Another factor considered as relevant in the present study was that approximately 75% of the cases had an interval of up to three days between the Doppler study and the labor, and in 50% the interval was one day. In the study developed by Baschat et al.(7) the mean interval between the last Doppler study and delivery has not been informed, while in other studies the mean interval was > 7 days(9,29). Variations in the Doppler study-delivery interval may explain differences in results, considering that severe alterations in the Doppler pattern of the umbilical and cerebral arteries precede the worsening in the fetal status(6) by 10-14 days. Prematurity remains as the single most important determinant of neonatal complications and mortality(9,27,28,30). In the literature, some authors have analyzed only premature fetuses, particularly at gestational ages < 32 weeks, differently from the cases in the present study, in which different gestational ages were included, allowing a separate analysis of outcomes in extremely premature neonates, premature neonates and term neonates, and evaluate the impact of prematurity on the perinatal outcomes(3,7,11,13). The change in results after adjustment for gestational age was significant. It is known that in cases where placental insufficiency and fetal hemodynamic alterations are diagnosed, the tendency is to interrupt the pregnancy to avoid intrauterine fetal death. Therefore, the association between alterations at Doppler and lower gestational ages is evident. Additionally, considering that the lower the gestational age is, the worst the perinatal outcomes are, it is understood that gestational age is a confusing variable in the study of the association between alterations at Doppler and perinatal outcomes. The most typical example is RDS. Before adjusting by gestational age, the Doppler alterations of the umbilical artery seemed to be associated with a six-time higher risk of RDS, but after the adjustment, this association was not significant. Among the studied adverse perinatal outcomes indicators, RDS is exactly the one more closely related to gestational age, more so than the situation of chronic intrauterine hypoxemia. It is therefore clear that the increase in risk of RDS in cases with alterations at Doppler is mostly due to the premature interruption of pregnancy induced by the Doppler result than the hypoxia condition of the fetus. It would be very attractive if the assessment of the fetal status were more important than the gestational age effects on perinatal outcomes, so that the moment of delivery could be based on the tests of fetal assessment. Therefore, the authors' opinion is that the gestational age should not be ignored in the analysis of the data evaluated in the present study. This is the most important contribution of the present study, and hopefully the publication of such results will contribute with future studies to confirm the relevance of the gestational age factor in their analyses to the performance of Doppler velocimetry for assessing fetal vitality.
REFERENCES 1. Sebire NJ. Umbilical artery Doppler revisited: pathophysiology of changes in intrauterine growth restriction revealed. Ultrasound Obstet Gynecol. 2003;21:419-22. [ ] 2. Campbell S, Pearce JM, Hackett G, et al. Qualitative assessment of uteroplacental blood flow: early screening for high-risk pregnancies. Obstet Gynecol. 1986;68:649-53. [ ] 3. Ozcan T, Sbracia M, d'Ancona RL, et al. Arterial and venous Doppler velocimetry in the severely growth-restricted fetus and associations with adverse perinatal outcome. Ultrasound Obstet Gynecol. 1998;12:39-44. [ ] 4. Nomura RMY, Francisco RPV, Sakamoto K, et al. Centralização da circulação fetal em gestações de alto risco: avaliação da vitalidade fetal e resultados perinatais. Rev Bras Ginecol Obstet. 2001;23:137-43. [ ] 5. Sebire NJ, Goldin RD, Regan L. Histomorphological evidence for chronic vasoconstriction of placental stem vessels in pregnancies with intrauterine growth restriction and abnormal umbilical artery Doppler velocimetry indices. J Pathol. 2001;195:19A. [ ] 6. Baschat AA, Gembruch U, Weiner CP, et al. Qualitative venous Doppler waveform analysis improves prediction of critical perinatal outcomes in premature growth-restricted fetuses. Ultrasound Obstet Gynecol. 2003;22:240-5. [ ] 7. Baschat AA, Galan HL, Bhide A, et al. Doppler and biophysical assessment in growth restricted fetuses: distribution of test results. Ultrasound Obstet Gynecol. 2006;27:41-7. [ ] 8. Soothill PW, Ajayi RA, Campbell S, et al. Relationship between fetal acidemia at cordocentesis and subsequent neurodevelopment. Ultrasound Obstet Gynecol.1992;2:80-3. [ ] 9. Bilardo CM, Wolf H, Stigter RH, et al. Relationship between monitoring parameters and perinatal outcome in severe, early intrauterine growth restriction. Ultrasound Obstet Gynecol. 2004;23: 119-25. [ ] 10. Hartung J, Kalache KD, Heyna C, et al. Outcome of 60 neonates who had ARED flow prenatally compared with a matched control group of appropriate-for-gestational age preterm neonates. Ultrasound Obstet Gynecol. 2005;25:566-72. [ ] 11. Hecher K, Bilardo CM, Stigter RH, et al. Monitoring of fetuses with intrauterine growth restriction: a longitudinal study. Ultrasound Obstet Gynecol. 2001;18:564-70. [ ] 12. Harman CR, Baschat AA, Gembruch U. Venous Doppler in IUGR. Which vessel? Which parameter? Am J Obstet Gynecol. 2001;185:53. [ ] 13. Ferrazzi E, Bozzo M, Rigano S, et al. Temporal sequence of abnormal Doppler changes in the peripheral and central circulatory systems of the severely growth-restricted fetus. Ultrasound Obstet Gynecol. 2002;19:140-6. [ ] 14. Schreuder AM, McDonnell M, Gaffney G, et al. Outcome at school age following antenatal detection of absent or reversed end diastolic flow velocity in the umbilical artery. Arch Dis Child Fetal Neonatal Ed. 2002;86:F108-14. [ ] 15. Baschat AA, Harman CR. Antenatal assessment of the growth restricted fetus. Curr Opin Obstet Gynecol. 2001;13:161-8. [ ] 16. Bernstein IM, Horbar JD, Badger GJ, et al. Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The Vermont Oxford Network. Am J Obstet Gynecol. 2000;182(1 Pt 1):198-206. [ ] 17. Zeitlin J, Ancel PY, Saurel-Cubizolles MJ, et al. The relationship between intrauterine growth restriction and preterm delivery: an empirical approach using data from a European case-control study. BJOG. 2000;107:750-8. [ ] 18. Yamamoto RM, Francisco RPV, Miyadahira S, et al. Fatores prognósticos para o óbito perinatal em gestações com diástole zero ou reversa na dopplervelocimetria das artérias umbilicais. Rev Bras Ginecol Obstet. 2000;22:353-63. [ ] 19. GRIT Study Group. A randomised trial of timed delivery for the compromised preterm fetus: short term outcomes and Bayesian interpretation. BJOG. 2003;110:27-32. [ ] 20. Francisco RPV, Nomura RMY, Miyadahira S, et al. Diástole zero ou reversa na dopplervelocimetria das artérias umbilicais. Rev Assoc Med Bras. 2001;47:30-6. [ ] 21. Andrade JQ, Miyadahira S, Nomura RMY, et al. Dopplervelocimetria dos compartimentos arterial e venoso da circulação fetal e umbilical em gestação de alto-risco: análise dos resultados perinatais. Rev Bras Ginecol Obstet. 2002;24:153-60. [ ] 22. Romero R, Kalache KD, Kadar N. Timing the delivery of the preterm severely growth- restricted fetus: venous Doppler, cardiotocography or the biophysical profile? Ultrasound Obstet Ginecol. 2002;19:118-21. [ ] 23. Pires P. Aplicações da dopplervelocimetria em gestação de alto risco. In: Pires P. Doppler no 2º e 3º trimestres da gestação & hemodinâmica feto-placentária. 1ª ed. Recife: Edupe; 2006. p. 67-82. [ ] 24. Pires P, Faundes A. Dopplervelocimetria na avaliação hemodinâmica materno-fetal. Femina. 2007;35:383-90. [ ] 25. Arduini D, Rizzo G. Normal values of pulsatility index from fetal vessels: a cross-sectional study on 1556 healthy fetuses.J Perinat Med. 1990;18: 165-72. [ ] 26. Schwarze A, Gembruch U, Krapp M, et al. Qualitative venous Doppler flow waveform analysis in preterm intrauterine growth-restricted fetuses with ARED flow in the umbilical artery - correlation with short-term outcome.Ultrasound Obstet Gynecol. 2005;25:573-9. [ ] 27. Baschat AA, Gembruch U, Reiss I, et al. Relationship between arterial and venous Doppler and perinatal outcome in fetal growth restriction. Ultrasound Obstet Gynecol. 2000;16:407-13. [ ] 28. Müller T, Nanan R, Rehn M, et al. Arterial and ductus venosus Doppler in fetuses with absent or reverse end-diastolic flow in the umbilical artery: correlation with short-term perinatal outcome. Acta Obstet Gynecol Scand. 2002;22:786-91. [ ] 29. Meyberg GC, Solomayer EF, Grischke EM, et al. Does the measurement of four fetal arteries provide more information than the measurement of just two arteries in prenatal Doppler sonography? Ultrasound Obstet Gynecol. 1999;13:407-14. [ ] 30. Zelop CM, Richardson DK, Heffner LJ. Outcomes of severely abnormal umbilical artery doppler velocimetry in structurally normal singleton fetuses. Obstet Gynecol. 1996;87:434-8. [ ] Received June 16, 2009. * Study developed at Faculdade de Ciências Médicas da Universidade de Pernambuco (UPE), Recife, PE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554