Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 1 - Jan. /Feb. of 2009
Vol. 42 nº 1 - Jan. /Feb. of 2009
|
ICONOGRAPHIC ESSAY
|
|
First trimester pregnancy abnormalities: iconographic essay |
|
|
Autho(rs): Lívia Teresa Moreira Rios, Ricardo Villar Barbosa de Oliveira, Marília da Glória Martins, Kemuel Pinto Bandeira, Olga Maria Ribeiro Leitão, Graciete Helena Nascimento Santos, Márcia Silva Sousa |
|
|
Keywords: Miscarriage, Pregnancy abnormalities, Transvaginal ultrasonography |
|
|
Abstract:
INTRODUCTION The clinical entity denominated as threatened miscarriage characterized by abnormal vaginal bleeding is common during early pregnancy, occurring in more than one third of pregnancies(1). Even in the presence of fetal heart activity, bleeding in the period between the 7th and 12th weeks is associated to 5–10% of gestational loss at the first trimester, particularly in cases occurring before the 9th week, and in cases where the mother's age is > 35 years(2,3). A relation between adverse gestational outcomes such as preterm premature rupture of membranes (PPROM) and preterm labor (PTL) has been reported in cases where the bleeding is observed at the second half of the third trimester of pregnancy(4). Transvaginal ultrasonography is the technique of choice for evaluating the gestational viability(5). Sonographic criteria for characterization of most conditions at the first gestational trimester are well established in the literature. A consensus is still to be reached in relation to the cut-off point to be adopted in the measurement of endometrial thickness for identifying the presence of retained gestational product. Diagnostic difficulties are usual in cases of early or partial gestational trophoblastic disease, when other diagnoses may be suggested. The present iconographic essay is aimed at demonstrating the main sonographic criteria already established in the literature that characterize most conditions at the first trimester of pregnancy, besides discussing their possible diagnostic difficulties.
PARTIAL OVULAR DETACHMENT The maternal circulation inside the placenta starts peripherally (in the placental margins) and is associated to physiological oxidative phenomena that may lead to membranes rupture and formation. The abnormal development of such membranes may result in subchorionic hemorrhage, enhancing the predisposition to an adverse gestational outcome at the third trimester (PPROM and PTL)(4). Such abnormality is common and also denominated as subchorionic hemorrhage or trophoblastic hematoma (Figure 1), being visualized in more than 18% of cases of threatened miscarriage. The presence of fetal heart activity confers an excellent prognosis(4,6). Clinically, subchorionic hemorrhage may course with vaginal bleeding. At ultrasonography, a crescent-shaped shadow is observed adjacent to the gestational sac, with debris. Gestational sac compression and consequential deformation may occur. In most of cases, a two-week follow-up evaluation confirms the hematoma resorption.
The main differential diagnosis for ovular detachment is incomplete fusion of parietal and capsular deciduas, whose texture is anechoic, homogeneous, as a function of the fluid collection in the space between the deciduas. As the gestational sac develops, the whole uterine cavity is occupied with the complete fusion of the capsular decidua, involving the gestational sac, with the parietal decidua that is the portion lining the uterine cavity wall. Thus, there is no sign of rectification of one of the gestational sac walls in this variation in abnormality that is frequently visualized at the first trimester and early in the second trimester of pregnancy (Figure 2).
The image identification at the first trimester brings confusion with ovular detachment, especially in the presence of vaginal bleeding.
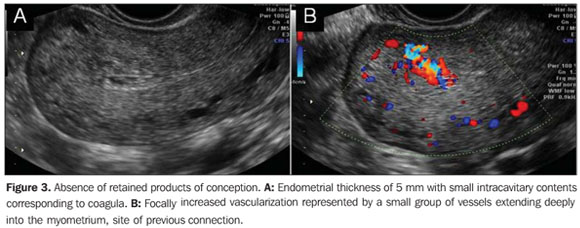
RETAINED PRODUCTS OF CONCEPTION In the literature, there is a great variation regarding the value to be adopted as measurement of the endometrial thickness for the diagnosis of retained products of conception in an incomplete miscarriage. Cut-off points between 8 and 15 mm have been adopted for differentiation between complete (Figure 3) and incomplete miscarriage (Figure 4), but such values still remain to be effectively validated(1).
Endometrial thickness < 15 mm, with no evidence of significant endometrial heterogeneity associated with absence of abdominal pain and cessation of the vaginal bleeding should be interpreted as complete miscarriage, without signs of retained products of conception(1,4). Retained products of conception are characterized by a thickened, disorganized and heterogeneous endometrium, with ill-defined mucosal layers and cavitary line, either with or without the presence of gestational sac. Clinically, the women presents abdominal pain and relative vaginal bleeding(1,4). In the presence of an intact gestational sac and closed cervix, the difficulty in a spontaneous resolution will be higher, requiring surgical evacuation(7).
EARLY EMBRYO DEATH Some sonographic findings characterize an embryo death in the first half of the first trimester in early phases, before the crown-rump length can be measured. The following aspects are highlighted: small, hyperechoic yolk sac (Figure 5), or hydropic yolk sac increased in volume with diameter > 7 mm, or even small amniotic cavity disproportionate to the gestational sac size. Before the 9th week, small gestational sac may be associated with aneuploidy (Figure 6)(4).
ANEMBRYONIC GESTATION At transvaginal ultrasonography, the yolk sac should be visualized in a gestational sac with mean diameter > 10 mm. The absence of a yolk sac within the gestational sac with > 10 mm in mean diameter, or the absence of a yolk sac within the gestational sac with > 16 mm in diameter characterize anembryonic gestation (Figure 7)(1,5).
GESTATIONAL TROPHOBLASTIC DISEASE The typical sonographic finding in most of cases of complete hydatidiform mole is a echogenic, intracavitary solid mass with intermingled, small cystic loci(8) resembling a "snow storm", corresponding to the vesicles that macroscopically characterize this condition. The higher the gestational age, the larger the vesicles visualized as homogeneous anechoic images, increasing the method specificity. The ultrasonography sensitivity will depend on the gestational age at the moment of the diagnosis. Ultrasonography can detect vesicles with > 2 mm in diameter (Figure 8). In early pregnancies with trophoblastic disease, the sonographic method accuracy is limited, hindering the differentiation of gestational trophoblastic disease from other conditions involving the endometrial cavity.
Partial hydatidiform mole offers higher diagnostic difficulty by ultrasonography. In a reasonable number of cases, this disease presents as an empty gestational sac corresponding to anembryonic gestation, or as early embryo death (Figure 9). However, two criteria have been described in the literature: gestational sac transverse/anteroposterior diameter ratio > 1,5 and cystic changes, irregularity of increase in echogenicity of decidual/placenta or myometrial reaction (Figure 10)(9).
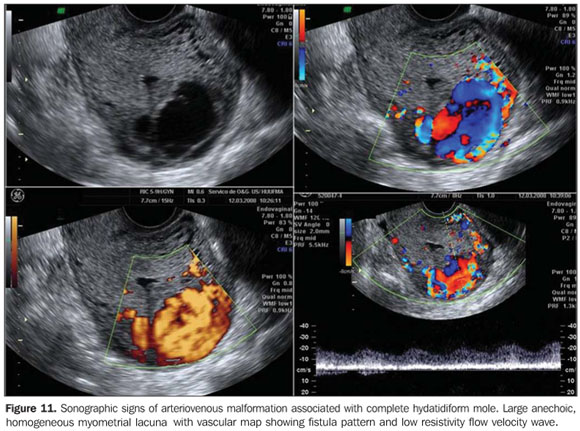
Myometrial nodules similar to intracavitary findings can be identified, demonstrating a low impedance flow velocity wave. Low resistivity indices are correlated with high levels of β-hCG. In cases of trophoblastic disease, velocimetric changes may precede by weeks the peak serum levels of β -hCG(10,11). Doppler US studies of the uterine arteries and of the myometrial lesion site must be performed. Uterine artery Doppler velocimetry is useful in the diagnosis, prognosis and follow-up of trophoblastic disease. In case of persistent disease, the vascular resistivity remains reduced in association with high hormone levels. On the other hand, color or amplitude Doppler US plays a significant role in facilitating the identification and determination of myometrial implants extent, besides allowing the diagnosis of arteriovenous malformations associated with trophoblastic disease that usually develop with low serum levels of β-hCG (Figure 11).
Despite the attempts to define the main sonographic findings of gestational trophoblastic disease, the gold standard in the diagnosis is the histopathological study of the product of conception following the surgical evacuation(9).
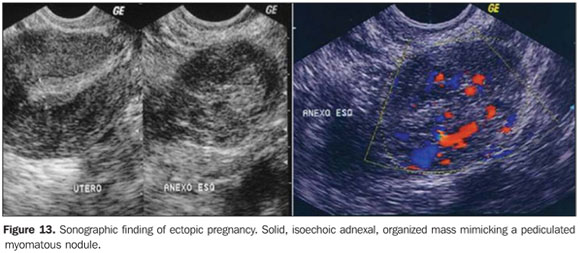
ECTOPIC PREGNANCY Sonographic findings of ectopic pregnancy will vary as a function of the gestational age and site. Classically, the following sonographic findings are described: tubal ring sign, adnexal disorganized mass molded to the adnexa and/or cul de sac, solid, organized mass with regular margins mimicking a pediculated myomatous nodule, clinically progressing with low β-hCG levels (Figures 12 and 13), and presence of a live extrauterine conceptus. Uncommon gestational sites may be observed such as abdominal ectopic pregnancy, cervical ectopic pregnancy and ectopic pregnancy in a previous Cesarean section pregnancy (Figure 14).
CONCLUSION First trimester obstetric abnormalities are identified by screening studies or in cases of abnormal vaginal bleeding with the objective of determining the gestation viability. In this context, transvaginal ultrasonography is the method of choice in the evaluation of first trimester pregnancy. In the presence of vaginal bleeding, this method is highly specific in the determination of the conceptus viability, most of times clearly defining the etiological process involved in the clinical condition. The knowledge of the sonographic findings that characterize each condition is essential for determining an appropriate clinical approach in these cases.
REFERENCES 1. Condous G, Okaro E, Bourne T. The conservative management of early pregnancy complications: a review of the literature. Ultrasound Obstet Gynecol. 2003;22:420–30. [ ] 2. Weiss JL, Malone FD, Vidaver J, et al. Threatened abortion: a risk factor for poor pregnancy outcome, a population-based screening study. Am J Obstet Gynecol. 2004;190:745–50. [ ] 3. Maso G, Piccoli M, D'Ottavio G, et al. OC017: Clinical significance of subchorionic haematoma in the first trimester of pregnancy. Ultrasound Obstet Gynecol. 2003;22(Suppl 1):4. [ ] 4. Jauniaux E, Johns J, Burton GJ. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet Gynecol. 2005;25:613–24. [ ] 5. Falco P, Zagonari S, Gabrielli S, et al. Sonography of pregnancies with first-trimester bleeding and a small intrauterine gestational sac without a demonstrable embryo. Ultrasound Obstet Gynecol. 2003;21:62–5. [ ] 6. Mantoni M. Ultrasound signs in threatened abortion and their prognostic significance. Obstet Gynecol. 1985;65:471–5. [ ] 7. Nielsen S, Hahlin M, Möller A, et al. Bereavement, grieving and psychological morbidity after first trimester spontaneous abortion: comparing expectant management with surgical evacuation. Hum Reprod. 1996;11:1767–70. [ ] 8. Benson CB, Genest DR, Bernstein MR, et al. Sonographic appearance of first trimester complete hydatidiform moles. Ultrasound Obstet Gynecol. 2000;16:188–91. [ ] 9. Fine C, Bundy AL, Berkowitz RS, et al. Sonographic diagnosis of partial hydatidiform mole. Obstet Gynecol. 1989;73(3 Pt 1):414–8. [ ] 10. Yacin O, Ozalp S, Tanir M. Assessment of gestational trophoblastic disease by Doppler ultrasonography. Eur J Obstet Gynecol Reprod Biol. 2002;103:83–7. [ ] 11. Oguz S, Sargin A, Aytan H, et al. Doppler study of myometrium in invasive gestational trophoblastic disease. Int J Gynecol Cancer. 2004;14: 972–9. [ ] Received July 28, 2009. * Study developed at Unit of Obstetrics and Gynecology, Hospital Universitário da Universidade Federal do Maranhão (HU-UFMA), São Luís, MA, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554