Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 2 - Mar. / Apr. of 2012
Vol. 45 nº 2 - Mar. / Apr. of 2012
|
CASE REPORT
|
|
Takotsubo cardiomyopathy following subarachnoid hemorrhage |
|
|
Autho(rs): Eduardo Wajnberg |
|
|
Keywords: Subarachnoid hemorrhage; Aneurysm; Takotsubo cardiomyopathy. |
|
|
Abstract: INTRODUCTION
Takotsubo syndrome corresponds to a cardiomyopathy characterized by a transient myocardial dysfunction affecting the left ventricular apex that classically occurs after major physical or emotional stress, and that is also called "broken heart syndrome" or stress-induced cardiomyopathy"(1). The authors report the case of a patient with takotsubo syndrome induced by subarachnoid hemorrhage. CASE REPORT A 55-year-old woman presented an episode of sudden and intense migraine with signs of Fisher grade 3 subarachnoid hemorrhage (Figure 1). After digital angiography, which revealed the presence of an anterior communicating aneurysm with 3 mm in diameter, the patient was submitted to endovascular treatment by embolization with platinum microcoils. In the postoperative period, the patient progressed with hemodynamic instability associated with left-sided heart failure and cardiogenic shock, requiring orotracheal intubation, mechanical ventilation, and use of inotropic and diuretic drugs. Electrocardiogram (ECG) revealed lateral ST segment elevation and long QT interval. Cardiac enzyme tests demonstrated slightly high troponin and CPK levels, and echocardiogram showed decreased left ventricular ejection fraction associated with apical akinesia and basal hypercontractility (Figure 2). The patient was referred for catheterization which did not revealed any significant atherosclerotic lesion. Ventriculography confirmed the ballooned appearance of the left ventricle, resembling the shape of an amphora characteristic of the syndrome (Figure 3). In about one week, the clinical condition of the patient progressively improved, the isotropic drugs dose was decreased, and the left ventricular function was recovered. 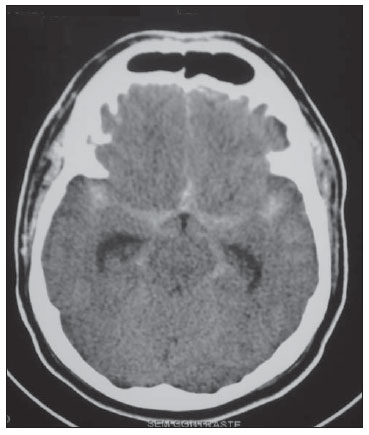 Figure 1. Cranial computed tomography revealing diffuse Fisher grade 3 subarachnoid hemorrhage and subtle ectasia of the temporal horns of lateral ventricles. 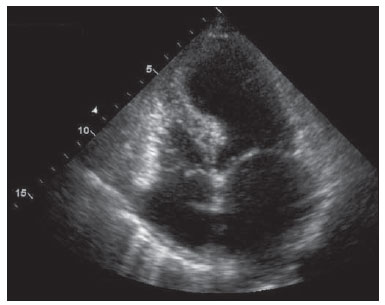 Figure 2. Echocardiography, coronal section, four-chamber view demonstrating the ballooned appearance of left ventricle. 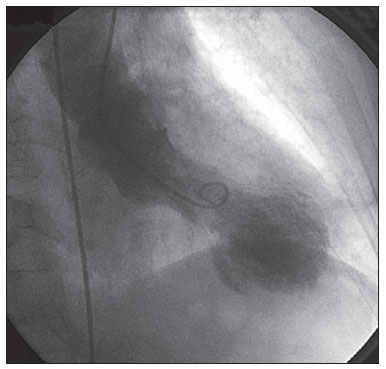 Figure 3. Ventriculography revealing the characteristic appearance of takotsubo syndrome: the amphora shape of the left ventricle at end systole. DISCUSSION Takotsubo syndrome, also called "transient left ventricular apical ballooning", was described in 1990 by Sato et al.(2). The name of this syndrome refers to the appearance of the left ventricle during end systole at ventriculography and its resemblance with the amphora-shaped octopus trap (corresponding to the Japanese term tako = octopus, tsubo = trap – Figure 4). A multifactorial etiology is probable, but certainly there is involvement of a failure in autoregulation of the myocardial microvasculature, transient coronary vasospasm and an abnormal response to catecholamines released as a reaction against stress(3). There is a marked predominance (82% to 100%) of this syndrome in women, particularly among those in the premenopausal period, with mean age between 62 and 75 years. 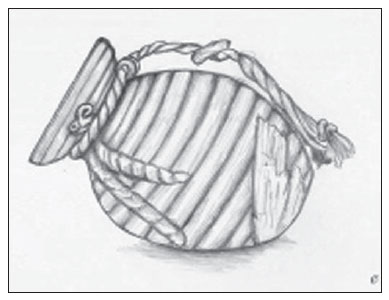 Figure 4. Drawing of the amphora utilized as octopus trap which characterizes the shape of the left ventricle at end systole, hence the name of the syndrome. Diagnostic criteria include the ballooning appearance of the ventricle at echocardiography or ventriculography, besides basal segments hypercontraction and alterations of the ST segment and T wave at ECG. In terms of clinical, biological and ECG features(4), the syndrome many times resembles acute myocardial infarction, but myocarditis and drug abuse, such as cocaine are also included in the differential diagnosis. The absence of significant coronary artery disease at cardiac catheterization must suggest the diagnosis of this syndrome and, if suspected, left ventriculography should be performed(5). The excessive release of catecholamines triggered by physical or emotional stress is proposed as the main underlying mechanism in the pathogenesis of this phenomenon, which in the present case is secondary to subarachnoid hemorrhage. Magnetic resonance imaging is a promising method for the diagnosis and assessment of this new entity, allowing the differentiation between irreversible lesion characterized by late gadolinium enhancement and myocardial edema(6). Thus, cardiac MRI can assess myocardial viability, constituting a relevant prognostic tool(7). Generally, it may be said that the prognosis of this disease is good, with complete myocardial contractility recovery after some days/ weeks(8,9). CONCLUSION Takotsubo syndrome is an increasingly recognized and diagnosed disease and, with the present case report, the authors highlight that it should be considered in the differential diagnosis of myocardial dysfunction occurring in the context of intracranial hemorrhages. Different imaging methods play a critical role in the diagnosis, and MRI plays a promising role in the assessment of this disease. REFERENCES 1. Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27:1523–9. 2. Sato H, Tateishi H, Uchida T, et al. Takotsubo type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M, editors. Clinical aspect of myocardial injury: from ischemia to heart failure. Tokyo: Kagaku Hyoronsha; 1990. p. 56– 64. [in Japanese]. 3. Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–48. 4. Bybee KA, Kara T, Prasad A, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004;141:858–65. 5. Azzarelli S, Galassi AR, Amico F, et al. Clinical features of transient left ventricular apical ballooning. Am J Cardiol. 2006;98:1273–6. 6. Fernández-Pérez GC, Aguilar-Arjona JA, de la Fuente GT, et al. Takotsubo cardiomyopathy: assessment with cardiac MRI. AJR Am J Roentgenol. 2010;195:W139–45. 7. Eitel I, Behrendt F, Sareban M, et al. The utility of cardiovascular magnetic resonance imaging in Takotsubo cardiomyopathy (apical ballooning) for differential diagnosis, pathophysiological insights and additional findings. J Cardiovasc Magn Res. 2009;11(Suppl 1):O23. 8. Sharkey SW, Windenburg DC, Lesser JR, et al. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–41. 9. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–17. MD, MSc, Hospital Universitário Clementino Fraga Filho – Universidade Federal do Rio de Janeiro (HUCFF-UFRJ), Rio de Janeiro, RJ, Brazil. Mailing Address: Dr. Eduardo Wajnberg Rua Nina Rodrigues, 72/102, Jardim Botânico Rio de Janeiro, RJ, Brazil, 22461-010 E-mail: eduardowj@gmail.com Received July 19, 2011. Accepted after revision September 22, 2011. Study developed at Hospital Universitário Clementino Fraga Filho – Universidade Federal do Rio de Janeiro (HUCFF-UFRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554