Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 6 - Nov. / Dec. of 2015
Vol. 48 nº 6 - Nov. / Dec. of 2015
|
ORIGINAL ARTICLE
|
|
Monte Carlo derivation of filtered tungsten anode X-ray spectra for dose computation in digital mammography |
|
|
Autho(rs): Lucas Paixão1; Bruno Beraldo Oliveira1; Carolina Viloria2; Marcio Alves de Oliveira3; Maria Helena Araújo Teixeira4; Maria do Socorro Nogueira5 |
|
|
Keywords: Mammography; X-ray spectra; HVL; Monte Carlo. |
|
|
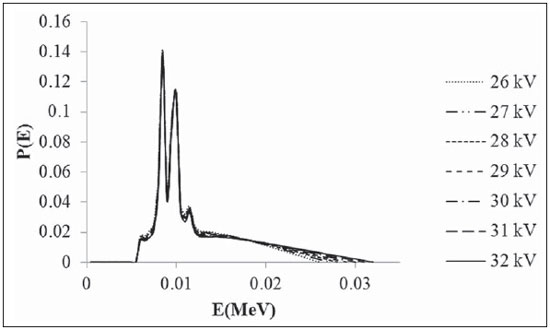
Abstract: INTRODUCTION
Radiographic breast imaging (mammography) is indicated for detection, diagnosis and clinical management of cancer. Moreover, mammography is the most widely used imaging modality for breast cancer screening(1). Breast dosimetry is an important part of the quality assurance program, provides means to define and verify the standards of good practice, besides contributing in the optimization of radiological protection(2,3). It is widely accepted that the mean glandular dose (DG) for the breast glandular tissue is the most useful magnitude for characterizing breast cancer risk(2,4). Because of the difficulty to measure it directly on the breast, the procedure to estimate the DG values consists in making use of conversion factors that relate incident air kerma (Ki) at this dose value. Generally, the conversion factors vary with the X-ray spectrum half-value layer (HVL) and the breast composition and thickness. By means of computer simulations, several authors have calculated such factors with the Monte Carlo method(5-8). The Monte Carlo radiation transport simulations are recognized as an important tool in dose calculations in different fields related to medical physics(9). Monte Carlo codes can be used in mammography to simulate and characterize photon beams produced; radiation dose absorbed by patient's organs; and dosimetry involving phantoms(10). Many X-ray spectral models for DG computer simulations purposes are available in the diagnostic range(11,12). One of the models available(13) generates polyenergetic X-ray spectra for molybdenum, rhodium, and tungsten anodes. The spectra produced by this model do not include any added filtration except by the 0.5 mm beryllium window of the X-ray tube and any self-filtration by the anode itself. The objective of the present study is to use Monte Carlo simulations to generate filtered X-ray spectra used in digital mammography systems from unfiltered spectra. Therefore, the Monte Carlo EGSnrc code package with the C++ class library (egspp) was employed to derive filtered tungsten X-ray spectra. Filtered spectra for rhodium filter were obtained for tube potentials between 26 and 32 kV. The HVLs of simulated filtered spectra were compared with those experimentally obtained with a solid state detector in a digital mammography system to validate the results. The results were also compared with the values recommended by the Technical Reports Series no. 457 of the International Atomic Energy Agency(14). MATERIALS AND METHODS Geometric model The geometric model adopted in the simulations was based on the Hologic Selenia Dimensions system (Hologic, Inc.; Bedford, MA) of a mammography clinic located in Belo Horizonte, MG, Brazil. A schematic drawing is shown on Figure 1. 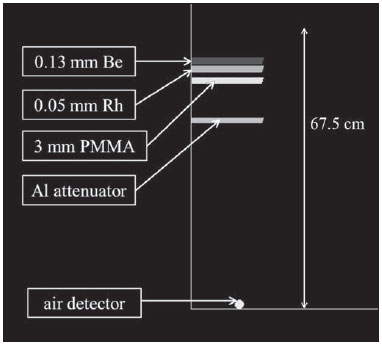 Figure 1. Geometric model schematic drawing. Such a mammography system has a focal spot of 0.3 mm, a 0.63 mm beryllium window and 0.050 mm rhodium filter. The distance between the breast support and the focal spot is 67.5 cm. Since the spectra have a 0.5 mm beryllium inherent filtration, to simulate the 0.63 mm beryllium window of clinical system, a 0.13 mm beryllium (ρ = 1.848 gcm-3) window was positioned at 5.0 cm from the focal spot in the simulations. The rhodium (ρ = 12.41 gcm-3) filter was modelled at 7 cm. Since the HVL measurements are performed in the presence of the compression plate, a polymethylmethacrylate (PMMA) compression plate was modelled with 18.0 × 24.0 × 0.3 cm3 at 10 cm(14). The aluminium (ρ = 2.6989 gcm-3) attenuators were positioned at 20 cm, with thicknesses ranging from 0.4 and 0.8 mm. All distances are relative to focal spot. An air (ρ = 0.00120479 gcm-3) sphere of 6 cm3 was centred laterally at 66.37 cm from the tube focal spot and at 6 cm from the chest wall edge as a detector. The breast support and X-ray scatter reduction grid were not modelled. The density and composition of materials utilized in the simulations were obtained in the material library of the EGSnrc code. Monte Carlo simulations The Monte Carlo EGSnrc code package(15) with the C++ class library (egspp) was employed(16). The unfiltered tungsten X-ray spectra for tube potentials between 26 and 32 kV (Figure 2) were simulated(13). The radiation beam was collimated into a rectangular shape of 1.13 cm side. Thus the collimated beam impinges directly on the modelled detector. Electrons and photons are followed down to a threshold energy of 10 keV. Bound Compton scattering, Electron Impact Ionization, Rayleigh scattering and atomic relaxations are turned on. NIST tabulations of differential bremsstrahlung cross sections and photon cross sections from XCOM tabulations are used(17). Absorbed dose in air simulations were performed for HVL calculations with 5 × 107 histories which represent a statistical error of about 3%. The simulations were performed in a personal computer with an Intel® Xeon® Quad CPU of 3.30 GHz with 4 GB RAM. HVL measurements Irradiations were carried out using the W/Rh target/filter combination and a Selenia Dimensions model Hologic DBT system using a direct radiography mode. Measurements were performed using a calibrated set manufactured by Unfors, composed of the solid state detector model 8202031-H Xi R/F & MAM Detector Platinum Series 181096, connected to the base unit model 8201023-C Xi Base unit Platinum Plus w mAs, Series 190046. The solid state detector sensitive volume was laterally centered at 65 cm from the tube focal spot and at 6 cm from the chest wall edge. The X-ray tube voltage was varied from 27 to 31 kV at intervals of 1 kV. The HVL values using the solid state detector were obtained directly by averaging three measurements in mmAl. All irradiations were done with a tube loading of 50 mAs. It is important to observe that irradiations were performed with the compression plate in contact with the detector (Figure 3). This was necessary for future use of the HVL values in the determination of DG conversion factors(6,18).  Figure 3. Experimental setup showing the compression plate in contact with detector. RESULTS The W/Rh target/filter combination X-ray spectra HVL values obtained by Monte Carlo simulations and experimentally are shown on Table 1. The experimental values for 26 and 32 kV were estimated from linear fitting of the remaining values. The uncertainty of all results was estimated to be 3% (1 σ). The estimated values uncertainty was < 3% but this value was maintained in order to be conservative. The experimental HVL values uncertainty calculation is shown on Table 2. The main sources of experimental values uncertainty are calibration (2%) and energy dependence (2%) of the detector. The HVL values obtained in the present study are also shown on Figure 4, along with HVL values recommended by TRS-457(14). Linear fitting of the data along with its equation and the R2 coefficient are also shown on Figure 4. For a better viewing, only experimental values uncertainty bars are shown. 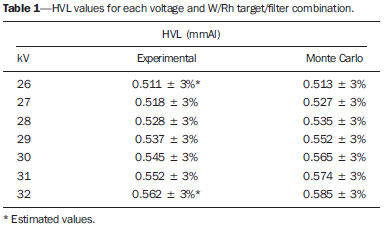 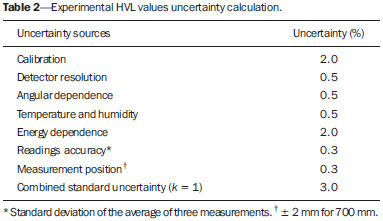 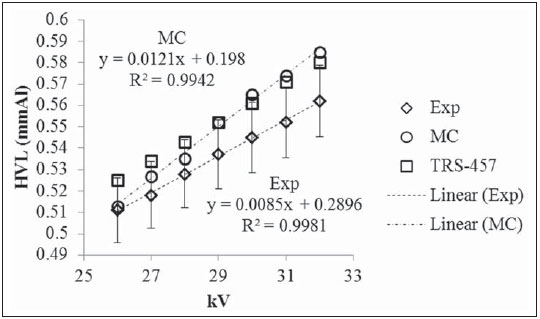 Figure 4. HVL values for each voltage and W/Rh target/filter combination. DISCUSSION Calculated HVL values showed good agreement as compared with those experimentally obtained. The highest relative percentage difference between the Monte Carlo calculated HVL values and experimental HVL values was 4%. Taking into account the values recommended by the TRS-457, the relative percentage difference for Monte Carlo calculated HVL values ranged between -2% and 1% and was -3% for all experimental values. Such Monte Carlo calculated HVL values are preliminary results. Great improvement has been achieved for both results and uncertainties by using Ki rather than absorbed dose in air. New results are reported by Paixão et al.(19). The results obtained in this study show that the EGSnrc Monte Carlo code generates the X-ray spectra with appropriate filtration. As an example, a Monte Carlo obtained W/Rh target/filter combination X-ray spectra for 29 kV is shown on Figure 5. The filtered tungsten anode X-ray spectra may be used for dosimetry studies in mammography. When using the filtered spectrum instead of the unfiltered spectrum in dose simulations, one may gain in computational time. 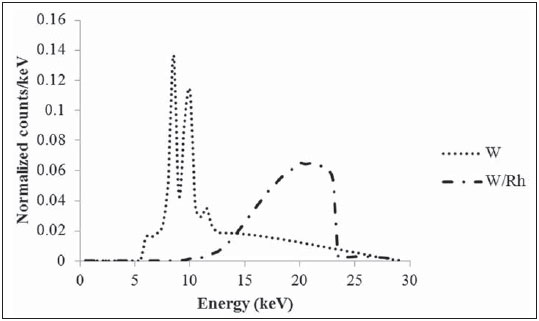 Figure 5. Tungsten target X-ray spectra(13) and Monte Carlo obtained W/Rh target/filter combination X-ray spectra for 29 kV. Although Mo/Mo target/filter is the most widely used combination in clinical practice, new combinations have been introduced with the increasing use of digital mammography systems(8). Therefore, the results of the present study are important as they can be applied to state of the art equipment. CONCLUSIONS In the present study, the Monte Carlo code EGSnrc was employed for simulation of filtered X-ray spectra used in digital mammography. The differences in the HVL values were less than 4% for all tube voltages. Such results demonstrate that the EGSnrc code provides a filtration of the raw X-ray spectra in good agreement with those experimentally determined. The W/Rh target/filter combination X-ray spectra obtained in the simulations may be used in future Monte Carlo simulations studies in digital mammography. Acknowledgments The authors are thankful to Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes) and to Comissão Nacional de Energia Nuclear (CNEN) for the incentive with PhD fellowships and to Dra. Maria Helena Araújo Teixeira Clinic for providing the DBT system. The present study was financially supported by Fundação de Amparo à Pesquisa do Estado de Minas Gerais (Fapemig) and Ministry of Science and Technology (MCT), Brazil, through the Brazilian Institute of Science and Technology (INCT) for Radiation Metrology in Medicine. REFERENCES 1. Chevalier M, Morán P, Ten JI, et al. Patient dose in digital mammography. Med Phys. 2004;31:2471-9. 2. International Commission on Radiation Units and Measurements. Mammography - assessment of image quality (ICRU Report 82). United Kingdom: ICRU; 2009. 3. Oliveira MA, Dantas MVA, Santana PC, et al. Assessment of glandular dose and image quality in mammography using computerised radiography employing a polymethylmetacrilate breast simulator. Radiat Meas. 2011;46:2081-5. 4. Dance DR, Skinner CL, Carlsson GA. Breast dosimetry. Appl Radiat Isot. 1999;50:185-203. 5. Wu X, Gingold EL, Barnes GT, et al. Normalized average glandular dose in molybdenum target-rhodium filter and rhodium target-rhodium filter mammography. Radiology. 1994;193:83-9. 6. Dance DR, Skinner CL, Young KC, et al. Additional factors for the estimation of mean glandular breast dose using the UK mammography dosimetry protocol. Phys Med Biol. 2000;45:3225-40. 7. Boone JM. Normalized glandular dose (DgN) coefficients for arbitrary X-ray spectra in mammography: computer-fit values of Monte Carlo derived data. Med Phys. 2002;29:869-75. 8. Dance DR, Young KC, van Engen RE. Further factors for the estimation of mean glandular dose using the United Kingdom, European and IAEA breast dosimetry protocols. Phys Med Biol. 2009;54:4361-72. 9. Rogers DWO. Fifty years of Monte Carlo simulations for medical physics. Phys Med Biol. 2006;51:R287-301. 10. Cassola VF, Hoff G. Comparative study of computational dosimetry involving homogeneous phantoms and a voxel phantom in mammography: a discussion on applications in constancy tests and calculation of glandular dose in patients. Radiol Bras. 2010;43:395-400. 11. Ay MR, Sarkar S, Shahriari M, et al. Assessment of different computational models for generation of x-ray spectra in diagnostic radiology and mammography. Med Phys. 2005;32:1660-75. 12. Cunha DM, Tomal A, Poletti ME. Monte Carlo simulation of x-ray spectra in mammography and contrast-enhanced digital mammography using the code PENELOPE. IEEE Trans Nucl Sci. 2013;60:495-502. 13. Boone JM, Fewell TR, Jennings RJ. Molybdenum, rhodium, and tungsten anode spectral models using interpolation polynomials with application to mammography. Med Phys. 1997;24:1863-74. 14. International Atomic Energy Agency. Dosimetry in diagnostic radiology: an international code of practice. Technical Reports Series no. 457. Vienna: IAEA; 2007. 15. Kawrakow I, Rogers D. The EGSnrc code system: Monte Carlo simulation of electron and photon transport. NRCC Report PIRS-701. Ottawa, Canada: National Research Council of Canada; 2010. 16. Kawrakow I, Mainegra-Hing E, Tessier F, et al. The EGSnrc C++ class library. National Research Council of Canada. Report PIRS-898 (Rev A); 2009. 17. Mainegra-Hing E, Kawrakow I. Efficient x-ray tube simulations. Med Phys. 2006;33:2683-90. 18. Dance DR. Monte Carlo calculation of conversion factors for the estimation of mean glandular breast dose. Phys Med Biol. 1990;35:1211-9. 19. Paixão L, Oliveira BB, Oliveira MA, et al. New method for generating breast models featuring glandular tissue spatial distribution. Submitted to Radiat Phys Chem on February 2015. 1. M.Sc., Post-graduation in Science and Technology of Radiations, Minerals and Materials - Centro de Desenvolvimento da Tecnologia Nuclear / Comissão Nacional de Energia Nuclear (CDTN/CNEN), Belo Horizonte, MG, Brazil 2. M.Sc., Post-graduation in Nuclear Sciences and Techniques - Departamento de Engenharia Nuclear da Universidade Federal de Minas Gerais (DEN-UFMG), Belo Horizonte, MG, Brazil 3. M.Sc., Professor, Department of Anatomy and Imaging, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil 4. MD, Radiologist, Technical Director, Clínica Dra. Maria Helena Araújo Teixeira, Belo Horizonte, MG, Brazil 5. D.Sc., Titular Researcher-Professor, Centro de Desenvolvimento da Tecnologia Nuclear / Comissão Nacional de Energia Nuclear (CDTN/CNEN), Departamento de Engenharia Nuclear da Universidade Federal de Minas Gerais (DEN-UFMG), Belo Horizonte, MG, Brazil Mailing Address: Lucas Paixão Centro de Desenvolvimento da Tecnologia Nuclear Avenida Presidente Antônio Carlos, 6627, Campus UFMG, Pampulha Belo Horizonte, MG, Brazil, 31270-901 E-mail: lucaspaixxao@hotmail.com Received October 12, 2014. Accepted after revision April 1, 2015. Study developed at Centro de Desenvolvimento da Tecnologia Nuclear / Comissão Nacional de Energia Nuclear (CDTN/CNEN), Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554