Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 55 nº 4 - July / Aug. of 2022
Vol. 55 nº 4 - July / Aug. of 2022
|
ORIGINAL ARTICLE
|
|
Uterine artery embolization with highly compressible calibrated microspheres for the treatment of uterine fibroids |
|
|
Autho(rs): Denis Szejnfeld1,a; Rômulo Florêncio Tristão Santos1,b; Antonio Massamitsu Kambara2,c; Marcelo Bueno de Oliveira Colli2,d; Felipe Nasser3,4,e; Mauricio de Sena Martins5,f; Suzan Menasce Goldman1,g |
|
|
Keywords: Leiomyoma; Uterine artery; Uterine artery embolization; Microspheres. |
|
|
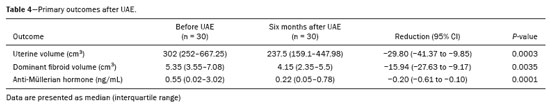
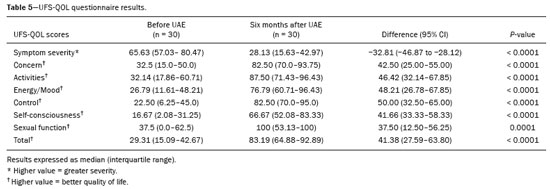
Abstract: INTRODUCTION
Uterine artery embolization (UAE) emerged as an alternative to hysterectomy in the 1990s(1–3). The procedure was based on well-established techniques for the treatment of pelvic bleeding related to trauma or gynecologic emergencies, such as postpartum hemorrhage, and later for the treatment of uterine fibroids. Since the initial reports, UAE has become a widely accepted, safe, and effective alternative to surgery(2–7), and it is now the leading minimally invasive treatment for symptomatic uterine fibroids(8). Initial studies have, for the most part, used polyvinyl alcohol particles as the embolic agent(9,10), demonstrating that the material is highly safe and effective. However, some technical difficulties related to microcatheter occlusion have prompted the use of calibrated spheres, with similar or even superior efficacy(10), notably attributed to the increased compressibility of the spheres, which enables them to pass through the microcatheter more easily and to settle better into the embolized vessels, allowing for more distal and consistent embolization. Embosoft calibrated microspheres (Scitech Medical, Aparecida de Goiânia, Brazil) were developed using Polifit 70 as a coating material, which allows a level of compressibility of approximately 40% with subsequent reexpansion and return to the original spherical shape without fragmentation or deformation, thus providing more effective embolization. The present study aimed to evaluate the safety and efficacy of UAE for the treatment of fibroids using Embosoft Polifit 70 microspheres. MATERIALS AND METHODS Study design This was a prospective multicenter study. The study was approved by the research ethics committees of the participating institutions and was registered at ClinicalTrials.gov (NCT03535610). All participants gave written informed consent. The gynecology departments of the participating institutions selected a collective total of 32 women between 18 and 50 years age with symptomatic uterine fibroids for treatment with UAE between January 2019 and March 2020. Once selected, the interventional radiology teams of the institutions invited the women to participate in the study. Patients with contraindications to magnetic resonance imaging (MRI), previous surgical treatment, and recent use of gonadotropin-releasing hormone analogues were excluded. Participants completed the Uterine Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire(11), underwent contrast-enhanced pelvic MRI, and were submitted to anti-Müllerian hormone measurement. Thereafter, participants underwent fibroid embolization with a well-established standard technique, using Embosoft Polifit 70 microspheres with sizes ranging from 300 µm to 900 µm. The standard microsphere size used in the study was 500–700 µm. However, in cases of adenomyosis, one or two syringes of 300–500 µm microspheres could be used on each side prior to embolization with 500–700 µm microspheres. Initially, up to four syringes (8 mL each) of 500–700 µm microspheres were used in each patient (approximately two per side) and, if additional material was still needed, the microsphere size was increased to 700–900 µm. If four syringes (8 mL) of 700–900 µm microspheres (approximately two per side) had been used and stasis had not been reached, Gelfoam could be used in order to achieve complete embolization. The standard protocol was bilateral embolization. However, unilateral embolization could be used if one uterine artery was dominant (because the other was tapered and was not irrigating the leiomyoma, because there was a single fibroid with unilateral irrigation, or because there was only a single uterine artery). Embolization was performed up to the endpoint, characterized by the “pruned tree” appearance. At six months after UAE, the participants again completed the UFS-QOL questionnaire and underwent contrast-enhanced pelvic MRI. The primary outcome measures were the efficacy and safety profile of Embosoft Polifit 70 microspheres in UAE. Secondary outcome measures included the reduction in uterine volume and largest fibroid volume at six months after UAE, as assessed by pelvic MRI, and the impact of embolization on quality of life and ovarian function. Data collection and statistical analysis Data were collected and managed using Research Electronic Data Capture tools(12) and analyzed in R version 2020(13). Descriptive statistics, including means and standard deviations, were used in order to summarize continuous variables. The data were analyzed at two time points: baseline and six months after UAE. Given the small sample size, the Wilcoxon test was used in order to analyze continuous variables. The level of statistical significance was set at p ≤ 0.05. RESULTS A total of 32 patients were included in the study, with a mean age of 40.9 years (range, 28–49 years). Of those 32 patients, 17 (53.1%) were mixed-race, nine (28.1%) were white, and six (18.8%) were black. The mean body weight was 77.5 ± 17.2 kg, and the mean body mass index was 29.7 ± 6.2 kg/m2. Fifteen patients (46.9%) were using oral hormonal contraceptives. Thirteen patients (40.6%) had no children, and 19 (59.4%) had children. Patient data are shown in Table 1. 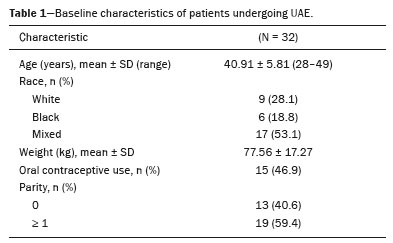 Eleven patients (34.4%) had regular menstrual cycles. The most commonly reported symptoms were abnormal uterine bleeding (in 81.3%), pelvic pain (in 81.3%), and compression (in 46.9%). Twelve patients (37.5%) had anemia due to abnormal uterine bleeding. Of the 32 patients, 10 (31.3%) had previously undergone pharmacologic fibroid treatment, five (15.6%) had previously undergone hysteroscopy, and one (3.1%) had previously undergone laparoscopy. The combination of uterine fibroids and adenomyosis was observed in 34.4% of the cases, in the focal form in 18.2% and in the diffuse form in 81.8%. Endometriosis accompanied by fibroids was observed in 6.3% of the cases. The mean number of fibroids seen on MRI was 6 (range, 1–16). Procedure-related data, such as type of anesthesia, arterial access site, intraprocedural medications, unilateral or bilateral embolization, and microsphere size, are shown in Table 2. Adverse events that occurred immediately after UAE and during follow-up are shown in Table 3.  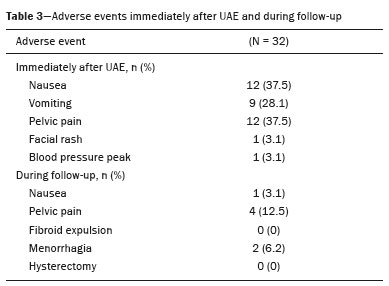 Of the 32 patients, 30 were reevaluated at six months after UAE. Two patients were lost to follow-up: one failed to return to the research center after UAE; and one dropped out of the study to undergo elective hysterectomy at another institution. Among the 30 patients who completed the study, we observed a median reduction of 21.4% in uterine volume and of 15.9% in dominant fibroid volume. Those results are shown in Table 4, together with the anti-Müllerian hormone levels. The UFS-QOL questionnaire results are shown in Table 5. DISCUSSION The use of UAE has gained acceptance as an alternative to myomectomy or hysterectomy in women with symptomatic uterine fibroids(14). Many women are satisfied with the results of this procedure, which include improvement of symptoms and a reduction in uterine volume, with preservation of the uterus and of fertility(7,8). The present study was designed to evaluate the short- and medium-term results of UAE using Embosoft Polifit 70 microspheres. In particular, the safety profile of the microspheres was objectively quantified based on adverse events, volume reductions (of the uterus and dominant fibroid), impact on quality of life, and impact on ovarian function. Safety issues are extremely important when using a new material, and verifying the absence of procedure- and material-related complications is the best way to ensure safety. In the present study, we found that UAE with Embosoft Polifit 70 microspheres resulted in a uterine volume reduction of 21.4% and dominant fibroid volume reduction of 15.9%. For comparison, Spies et al.(9) and Spies et al.(10) evaluated the same outcomes after UAE with tris-acryl gelatin microspheres, polyvinyl alcohol particles, and spherical polyvinyl alcohol, finding uterine volume reductions of 27.4%, 30.2%, and 16.4%, respectively, and dominant fibroid volume reductions of 39.0%, 42.5%, and 29.6%, respectively. Siskin et al.(15) evaluated uterine volume and dominant fibroid volume after embolization with tris-acryl gelatin microspheres and spherical polyvinyl alcohol, finding a uterine volume reduction of 12.6% and 16.5%, respectively, and a dominant fibroid volume reduction of 18.0% and 26.2%, respectively. Complication rates were similar across all studies(9,10,15). Comparing different embolic agents, Siskin et al.(15) reported percentage reductions in uterine volume and in dominant fibroid volume similar to those found in the present study. However, Spies et al.(9) and Spies et al.(10) reported reductions in uterine and dominant fibroid volumes greater than those observed in our sample. All operators were very careful to ensure that the endpoint was achieved; that is, that the embolization was complete and stable. Improvement in fibroid-related clinical symptoms after UAE is the most important measure of clinical efficacy(16). In addition to operator skill, the characteristics of the material employed have a direct impact on the level of fibroid devascularization achieved(16–18). One major concern is the recurrence of fibroid growth and symptoms over the long term. To our knowledge, there have been no definitive studies assessing fibroid recurrence, and it therefore remains unknown what the rate would be(9). In the present study, patients were followed for six months after UAE. Future studies could assess the degree of fibroid devascularization and rate of fibroid recurrence over longer periods. In the present study, we identified no adverse events that could be attributed to the material itself, although there were events attributed to the UAE procedure in general. Although fibroid expulsion after UAE has been reported to occur in 1.7–50.0% of cases(19), that complication was not observed in our sample. Our study has some limitations, including the medium-term clinical follow-up and the relatively small sample size. It has been well established that UAE produces consistent results in terms of symptom resolution. Although not recommended as a first-line therapy in patients who plan to become pregnant, UAE has a wide range of indications in women of reproductive age, which has generated great interest in its potential impact on female fertility(20,21). In summary, UAE using Embosoft Polifit 70 microspheres showed satisfactory results for the treatment of uterine fibroids, as well as demonstrating safety and efficacy. The procedure provides a reduction in uterine and dominant fibroid volumes, has a low rate of adverse events, and improves quality of life. REFERENCES 1. Ravina JH, Herbreteau D, Ciraru-Vigneron N, et al. Arterial embolisation to treat uterine myomata. Lancet. 1995;346:671–2. 2. Costantino M, Lee J, McCullough M, et al. Bilateral versus unilateral femoral access for uterine artery embolization: results of a randomized comparative trial. J Vasc Interv Radiol. 2010;21:829–35. 3. Manyonda I, Belli AM, Lumsden MA, et al. Uterine-artery embolization or myomectomy for uterine fibroids. N Engl J Med. 2020; 383:440–51. 4. Abbara S, Nikolic B, Pelage JP, et al. Frequency and extent of uterine perfusion via ovarian arteries observed during uterine artery embolization for leiomyomas. AJR Am J Roentgenol. 2007;188:1558–63. 5. American College of Obstetricians and Gynecologists. ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008;112(2 Pt 1):387–400. 6. Stokes LS, Wallace MJ, Godwin RB, et al. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomas. J Vasc Interv Radiol. 2010;21:1153–63. 7. Smeets AJ, Nijenhuis RJ, van Rooij WJ, et al. Uterine artery embolization in patients with a large fibroid burden: long-term clinical and MR follow-up. Cardiovasc Intervent Radiol. 2010;3:943–8. 8. Hu NN, Kaw D, McCullough MF, et al. Menopause and menopausal symptoms after ovarian artery embolization: a comparison with uterine artery embolization controls. J Vasc Interv Radiol. 2011;22: 710–5. 9. Spies JB, Allison S, Flick P, et al. Polyvinyl alcohol particles and tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: results of a randomized comparative study. J Vasc Interv Radiol. 2004;15:793–800. 10. Spies JB, Allison S, Flick P, et al. Spherical polyvinyl alcohol versus tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: results of a limited randomized comparative study. J Vasc Interv Radiol. 2005;16:1431–7. 11. Brito LGO, Malzone-Lott DA, Fagundes MFS, et al. Translation and validation of the Uterine Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire for the Brazilian Portuguese language. Sao Paulo Med J. 2017;135:107–15. 12. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. 13. The R Foundation. The R Project for Statistical Computing. [cited 2021 May 26]. Available from: https://www.R-project.org. 14. White AM, Banovac F, Spies JB. Patient radiation exposure during uterine fibroid embolization and the dose attributable to aortography. J Vasc Interv Radiol. 2007;18:573–6. 15. Siskin GP, Beck A, Schuster M, et al. Leiomyoma infarction after uterine artery embolization: a prospective randomized study comparing tris-acryl gelatin microspheres versus polyvinyl alcohol microspheres. J Vasc Interv Radiol. 2008;19:58–65. 16. Stampfl U, Radeleff B, Sommer C, et al. Midterm results of uterine artery embolization using narrow-size calibrated embozene microspheres. Cardiovasc Intervent Radiol. 2011;34:295–305. 17. Smeets AJ, Nijenhuis RJ, van Rooij WJ, et al. Embolization of uterine leiomyomas with polyzene F-coated hydrogel microspheres: initial experience. J Vasc Interv Radiol. 2010;21:1830–4. 18. Scheurig-Muenkler C, Wagner M, Franiel T, et al. Effect of uterine artery embolization on uterine and leiomyoma perfusion: evidence of transient myometrial ischemia on magnetic resonance imaging. J Vasc Interv Radiol. 2010;21:1347–53. 19. Shlansky-Goldberg RD, Coryell L, Stavropoulos SW, et al. Outcomes following fibroid expulsion after uterine artery embolization. J Vasc Interv Radiol. 2011;22:1586–93. 20. Kaump GR, Spies JB. The impact of uterine artery embolization on ovarian function. J Vasc Interv Radiol. 2013;24:459–67. 21. Fornazari VAV, Szejnfeld D, Szejnfeld J, et al. Evaluation of uterine contractility by magnetic resonance imaging in women undergoing embolization of uterine fibroids. Cardiovasc Intervent Radiol. 2019;42:186–94. 1. Escola Paulista de Medicina da Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 2. Instituto Dante Pazzanese de Cardiologia, São Paulo, SP, Brazil 3. Hospital Santa Marcelina, São Paulo, SP, Brazil 4. Hospital Israelita Albert Einstein, São Paulo, SP, Brazil 5. Hospital Maternidade Leonor Mendes de Barros, São Paulo, SP, Brazil a. https://orcid.org/0000-0001-8482-5955 b. https://orcid.org/0000-0002-8679-7369 c. https://orcid.org/0000-0001-6551-1942 d. https://orcid.org/0000-0002-6524-8176 e. https://orcid.org/0000-0001-6682-2259 f. https://orcid.org/0000-0001-8762-9204 g. https://orcid.org/0000-0002-3596-3419 Correspondence: Dr. Denis Szejnfeld Departamento de Diagnóstico por Imagem – EPM-Unifesp Rua Napoleão de Barros, 800, Vila Clementino São Paulo, SP, Brazil, 04024-002 Email: denis.cura@gmail.com Received 21 July 2021 Accepted after revision 7 October 2021 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554