Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 6 - Nov. / Dec. of 2014
Vol. 47 nº 6 - Nov. / Dec. of 2014
|
CASE REPORT
|
|
Urachal neoplasia: a case report |
|
|
Autho(rs): Célio Lúcio Palha da Cruz1; Gabriel Lacerda Fernandes1; Marcelo Ricardo Canuto Natal2; Thales Roberto Teixeira Taveira1; Patrícia Amaral Bicalho3; Yanna Quitéria Iida Pimentel de Brito4 |
|
|
Keywords: Carcinoma; Urachus; Hematuria; Neoplasms of the bladder. |
|
|
Abstract: INTRODUCTION
The urachus, or median umbilical ligament, is a midline tubular structure extending from the apex of the bladder to the umbilicus. It is a vestigial remnant from at least two embryonic structures: the cloaca that is the cephalic extension of the urogenital sinus (a precursor of the fetal bladder), and the allantois, a derivative of the yolk sac. Urachal remnant diseases are uncommon and usually present either with nonspecific abdominal signs or urinary symptoms(1-4). The most common clinical finding in such diseases is hematuria that is present in up to 80% of cases. Other irritative-type signs and symptoms include dysuria, mictional frequency and urgency (40-50%) and suprapubic pain (70%). Urachal carcinomas tend to be more frequently found in men (2:1), in the age range between 40 and 70 years(1-3,5). Risk factors are still poorly defined and it is not clear whether carcinogens in the bladder play any role as in the case of urothelial carcinoma(3). Complications resulting from the presence of urachal remnants include infection and malignization. Clinically, such neoplasias are insidious and usually lead to a delay in their diagnosis. Thus, they frequently present a poor prognosis(1,6). CASE REPORT A female, 62-year-old patient presented with painless macroscopic hematuria for three years. Physical examination did not reveal any abnormality. The patient presented altered renal function, with urea 37 mg/dl, creatinine 1.6 mg/dl, 24-hour proteinuria 675 mg/1500 ml, type I urine with proteinuria (++), hematuria (30/field), leukocyturia (20/field). Ultrasonography (US) demonstrated heterogeneous, irregular, focal thickening on the bladder roof (Figure 1). Abdominal computed tomography (CT) demonstrated the presence of urachal remnant and expansile lesion on the midline of the meso hypogastrium region, with heterogeneous contrast enhancement on the transition point between the bladder and the urachus, suggesting neoplasia (Figures 2 and 3). Additionally, the patient presented multiple pulmonary nodules suggestive of metastasis (chest CT whose images are not included in the present report). Cystoscopy identified topical urethral meatus as a cleft, and absence of urine drainage through the left urethral meatus. Presence of a large vegetative lesion on the vesical dome (Figure 4). Biopsy revealed urachal squamous cell adenocarcinoma. 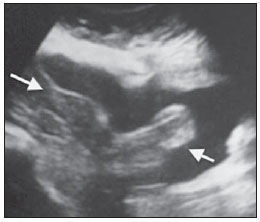 Figure 1. Ultrasonography, sagittal plane showing the presence of a remnant urachus and expansile, heterogeneous and irregular lesion (between arrows) at the midline of the meso hypogastrium region on the posterosuperior bladder wall. 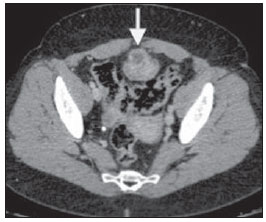 Figure 2. Computed tomography, axial section showing urachal remnant and a mass with soft parts components with heterogeneous contrast enhancement in the meso hypogastrium region at the anterosuperior midline for the apex of the bladder (arrow). 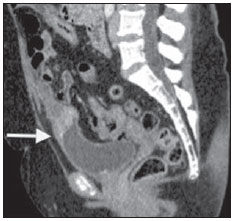 Figure 3. Computed tomography, sagittal reconstruction showing urachal remnant and expansile lesion on the midline of the meso hypogastrium region, with heterogeneous contrast enhancement on the transition point between the bladder and the urachus (arrow). 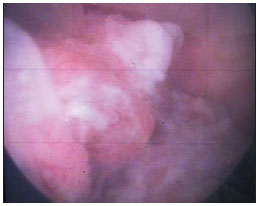 Figure 4. Cystoscopy (photography) identifying the presence of a large vegetative lesion on the vesical dome. The patient was submitted to chemotherapy on an outpatient basis and progressed with deep venous thrombosis of lower limbs and respiratory insufficiency and died some time afterwards. DISCUSSION Urachal carcinoma is extremely uncommon and most of times it presents itself as a lethal disease. Although the urachus is normally formed of transitional epithelium, most tumors (90%) are represented by adenocarcinomas. Most urachal adenocarcinomas are of the mucinous type, but even less common histological types are found, namely, transitional cell carcinomas, squamous cell carcinomas, small cell carcinomas and sarcomas(1,2,6). At US, the lesion is seen as a thickening of the anterior bladder wall, in many cases in contact with the anterior abdominal wall(3,5). At CT, urachal carcinoma appears as an anterosuperior mass extending from the midline to the apex of the bladder, with components of low attenuation which may represent areas of mucinous accumulation at pathological analysis. Peripheral calcifications occur in 50-70% of cases and are considered as pathognomonic for urachal adenocarcinoma(1,2,5). At magnetic resonance imaging (MRI), high signal intensity is observed on T2-weighted sequences due to the presence of mucin within the tumor. Additionally, MRI is an excellent tool in the staging of the disease(2). Radiological differential diagnoses include non-urachal adenocarcinomas, transitional cell carcinomas, infected urachal remnants, and metastasis from primary lesions of the colon, prostate or female genital tract(1,2,4). The literature identifies three types of urachal tumor staging systems: Sheldon, Henly and Ontario. Sheldon and Henly system are highlighted, and the Henly system is the most simplified one, that was later modified by the Mayo Clinic(7). Therefore, despite the rarity and diverse clinical presentations of urachal adenocarcinoma, the assisting physician must ever be attentive to patients with hematuria, suprapubic pain and imaging findings of thickening of the vesical dome(7). The main treatment for urachal adenocarcinoma is surgical resection. Chemotherapy has been reserved for cases of metastatic disease or local recidivation, and no evidence of clinical benefit from radiotherapy in the management of urachal adenocarcinoma has been reported in the literature(2,3,6,8). REFERENCES 1. Yu JS, Kim KW, Lee HJ, et al. Urachal remnant diseases: spectrum of CT and US findings. Radiographics. 2001;21:451-61. 2. Koster IM, Cleyndert P, Giard RW. Best cases from the AFIP: urachal carcinoma. Radiographics. 2009;29:939-42. 3. Ashley RA, Inman BA, Sebo TJ, et al. Urachal carcinoma: clinicopathologic features and long-term outcomes of an aggressive malignancy. Cancer. 2006;107:712-20. 4. Donate Moreno MJ, Giménez Bachs JM, Salinas Sánchez AS, et al. Patología del uraco: revisión de conjunto y presentación de tres casos. Actas Urol Esp. 2005;29:332-6. 5. Thali-Schwab CM, Woodward PJ, Wagner BJ. Computed tomographic appearance of urachal adenocarcinomas: review of 25 cases. Eur Radiol. 2005;15:79-84. 6. Oliveira C, Silva CB, Quinta A, et al. Carcinoma do úraco. Acta Urológica. 2009;26:164. 7. Krebs RK, Zylbersztejn DS, Manzano J, et al. Adenocarcinoma de úraco. In: Ortiz V, Srougi M, editores. Sinopse de urologia - Disciplina de Urologia da Escola Paulista de Medicina. São Paulo, SP: Grupo Editorial Moreira Júnior; 2008. p. 48-51. 8. Esteves FP, Pinto AC, Pinto AFC. Urachal adenocarcinoma. Braz J Urol. 2001;27:560-2. 1. MDs, Residents of Radiology and Imaging Diagnosis, Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil 2. MD, Radiologist, Medical Residency Coordinator (Radiology and Imaging Diagnosis), Hospital de Base do Distrito Federal (HBDF), Radiologist at Diagnóstico das Américas (DASA/Exame-Pasteur), Brasília, DF, Brazil 3. Medical Practice Resident Physician, Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil 4. Family and Community Physician - UBS Alvorada, Novo Gama, GO, Brazil Mailing Address: Dr. Célio Lúcio Palha da Cruz SQSW 306, ap. 509, Setor Sudoeste Cruzeiro, DF, Brazil, 70673-432 E-mail: celiolucio@hotmail.com Received August 10, 2013. Accepted after revision January 10, 2014. Study developed at Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554